Table of Contents
Overview – Coeliac Disease
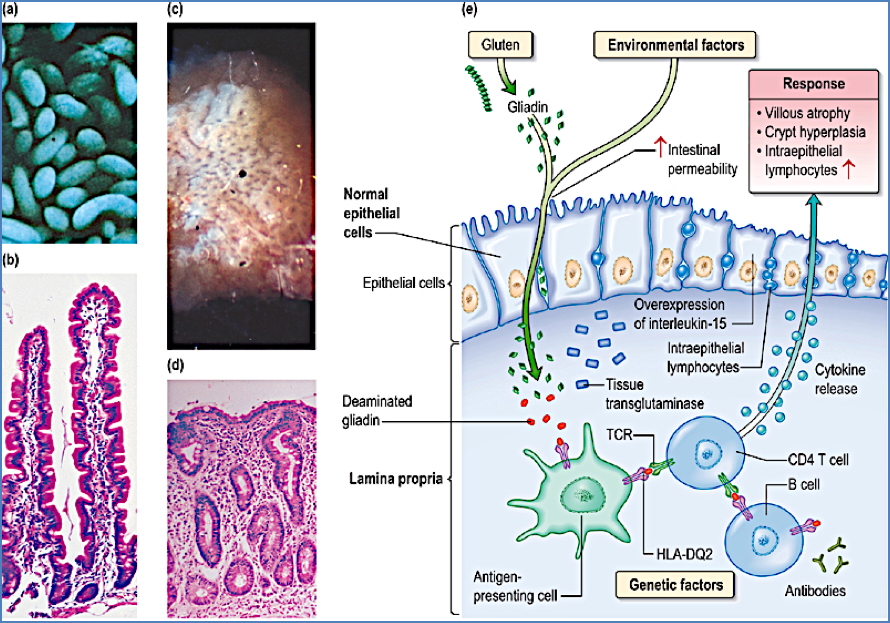
Coeliac disease is a chronic immune-mediated disorder triggered by gluten ingestion, primarily affecting the proximal small intestine. It leads to villous atrophy, crypt hyperplasia, and malabsorption, with wide-ranging clinical manifestations from fatigue to diarrhoea, weight loss, and nutrient deficiencies. Diagnosis involves both serological markers and duodenal biopsy, and management centres on strict lifelong adherence to a gluten-free diet. This page covers the essential pathology, clinical features, investigations, and treatment of coeliac disease for final-year medical students.
Definition
- Immune-mediated inflammatory disorder of the proximal small bowel triggered by gluten (specifically the prolamin fraction).
- Causes villous atrophy, malabsorption, and associated systemic symptoms.
Aetiology
- Genetic predisposition with HLA-DQ2/DQ8 association.
- Immunological reaction to gluten and related prolamins found in:
- Wheat
- Barley
- Rye
Pathophysiology
- Gluten ingestion → immune activation → chronic mucosal inflammation.
- Inflammation results in:
- Villous atrophy
- Crypt hyperplasia
- Loss of absorptive surface area in the small intestine → malabsorption.
Morphology
- Most marked in the proximal small bowel (duodenum and jejunum).
- Histological features:
- Flattened mucosa
- Absence or blunting of villi
- Crypt hyperplasia
- Infiltration with intraepithelial lymphocytes
Clinical Features
Epidemiology
- Can present at any age, but peaks:
- In infancy
- In 5th–6th decade of life
- More common in females
Symptoms and Signs
- General: Fatigue, malaise, weight loss
- Gastrointestinal:
- Diarrhoea or steatorrhoea
- Constipation (less common)
- Abdominal discomfort, pain, or bloating
- Extraintestinal:
- Angular stomatitis, mouth ulcers
- Nutritional deficiencies (e.g. iron, B12, folate)
Investigations
- Duodenal biopsy (gold standard):
- Confirms villous atrophy and crypt hyperplasia
- Serology:
- Anti-tissue transglutaminase (anti-tTG) IgA antibodies (highly sensitive)
- Anti-endomysial antibodies (EMA)
- Consider total IgA levels to exclude IgA deficiency
Management
- Strict lifelong gluten-free diet:
- Complete avoidance of wheat, rye, barley
- Nutritional supplementation:
- Iron, folate, calcium, vitamin D, and fat-soluble vitamins
- Monitoring:
- Antibody titres for compliance
- Repeat biopsy if symptoms persist
- Future:
- Enzyme replacement therapy (under research)
Complications
- Ulcerative jejunitis:
- Presents with fever, abdominal pain, bleeding, risk of perforation
- Malignancy:
- Increased risk of small bowel adenocarcinoma and enteropathy-associated T-cell lymphoma
- Bone disease:
- Osteomalacia → osteoporosis (due to calcium and vitamin D malabsorption)
- Increased risk of inflammatory bowel diseases
Differential Diagnosis
- Lactose intolerance
- Irritable bowel syndrome (IBS)
- Crohn’s disease
- Tropical sprue
Summary – Coeliac Disease
Coeliac disease is an autoimmune enteropathy triggered by gluten, leading to villous atrophy and malabsorption. It may present with gastrointestinal or systemic symptoms and is diagnosed via serology and duodenal biopsy. Management is based on a lifelong gluten-free diet and monitoring for nutritional deficiencies. For more related GI topics, visit our Gastrointestinal Overview page.