Table of Contents
Overview
Hepatitis refers to inflammation of the liver, commonly caused by viral infections, alcohol, toxins, or autoimmune processes. It is a critical topic for medical students due to its progression pathway — from acute or chronic inflammation to cirrhosis and eventually hepatocellular carcinoma. Understanding the distinct forms of hepatitis, from viral subtypes (A–E) to toxic causes like alcohol and paracetamol, is essential for early diagnosis, prevention, and effective management. This guide outlines the mechanisms, clinical patterns, and long-term consequences of hepatitis.
Definition
Hepatitis is defined as inflammation of the liver, which can be acute or chronic and is caused by viral, autoimmune, toxic, or metabolic insults.
Aetiology
Viral
- Hepatitis A–E (transmission and chronicity vary by type)
Toxic
- Alcoholic hepatitis
- Paracetamol overdose
Autoimmune
Other infectious agents
- EBV, CMV, HSV, Yellow Fever, Toxoplasmosis
Pathogenesis
Viral-Induced
- Hep A & E: Direct cytopathic effect, faecal-oral spread, acute only
- Hep B & D: Immune-mediated hepatocyte destruction
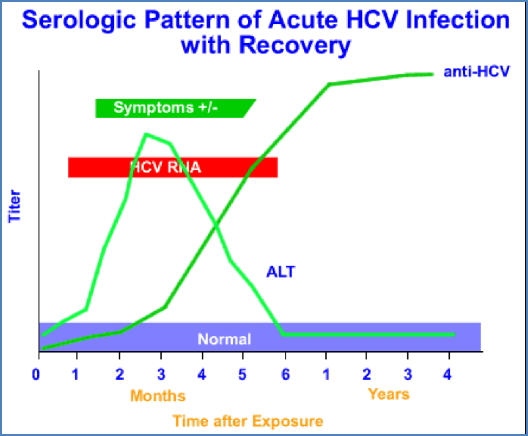
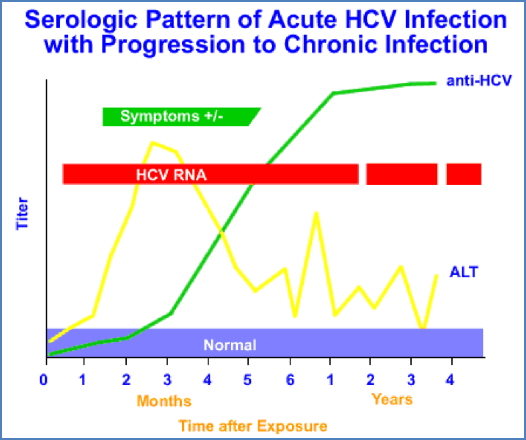
- Hep C: Chronic low-grade inflammation, not directly cytopathic
Toxin-Induced
- Alcohol: Acetaldehyde causes hepatotoxicity
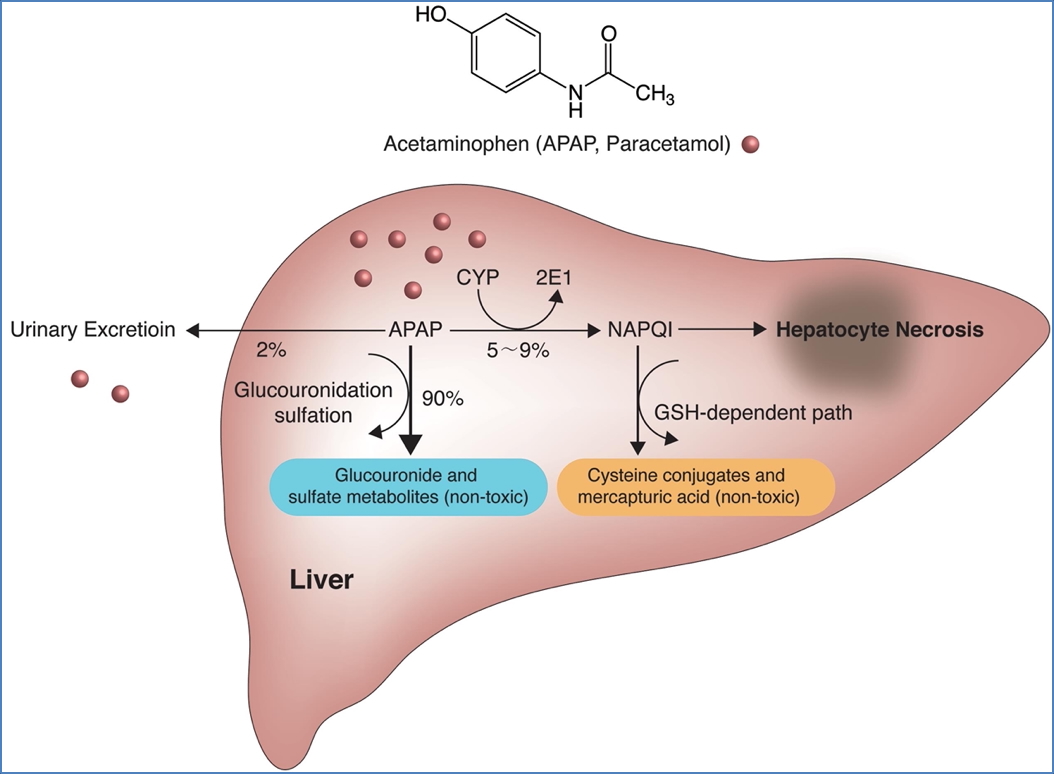
- Paracetamol: Glutathione depletion leads to centrilobular necrosis

Other
- EBV/CMV/HSV: secondary to other systemic viral infections
- Toxoplasmosis: Mimics mononucleosis, with mild hepatitis
Clinical Features
General Symptoms
- Fatigue, jaundice, anorexia, fever, malaise, arthralgia
- RUQ pain or hepatomegaly
Specific Findings
- Alcoholic Hepatitis: Dupuytren’s contracture, truncal ataxia, hepatic flap, Wernicke-Korsakoff
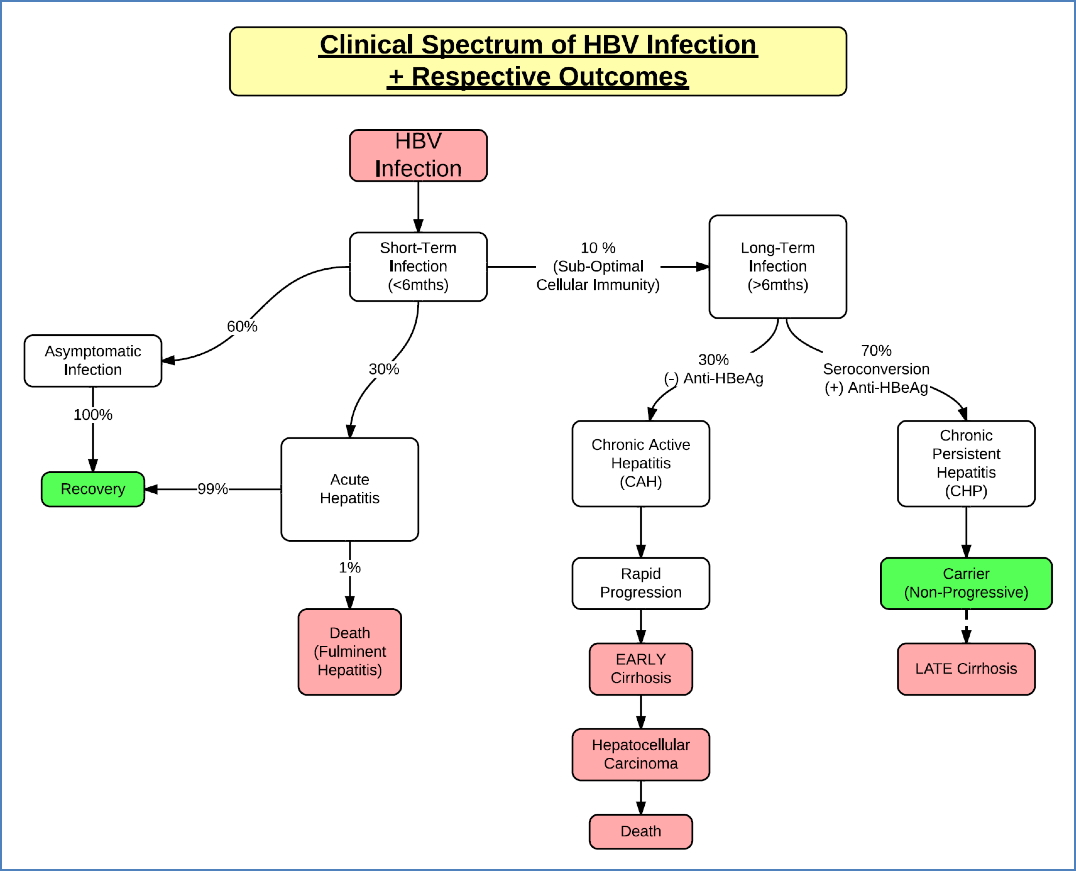
- Hep B: Variable chronicity; jaundice, pruritus, liver failure signs
- Hep C: Often asymptomatic until late; cirrhosis, HCC
- Hep D: Co-infection with Hep B; more severe course
- Hep A/E: Self-limiting; jaundice, cholestasis signs
- Paracetamol toxicity: Confusion, ALOC, rapid progression to liver failure
- Others: EBV/CMV – mild hepatitis in immunocompromised
Investigations
- LFTs: ALT/AST, GGT, ALP, bilirubin
- Serologies & PCR:
- Hep A–E viral panels
- Anti-HCV, HCV-RNA
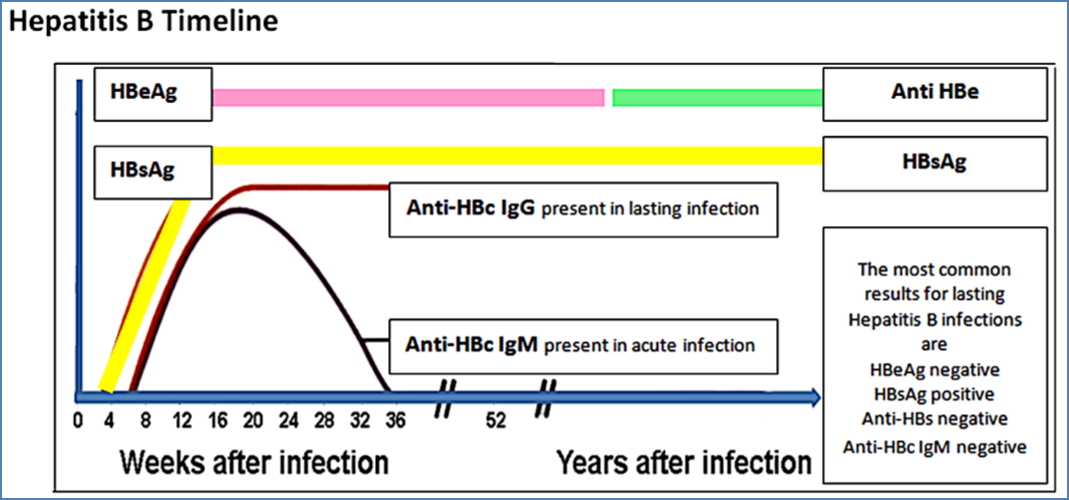
- HBsAg, Anti-HBs, Anti-HBc, HBeAg
- Paracetamol levels (in overdose)
- Imaging: For hepatomegaly, fibrosis, cirrhosis
- Liver biopsy: Occasionally indicated
Management
General
- Supportive care (fluids, nutrition, rest)
- Avoid hepatotoxic substances
Specific Treatments
- Alcoholic Hepatitis: Abstinence, thiamine + B12, diazepam
- Paracetamol Overdose: N-acetylcysteine (based on nomogram)
- Hep B: IFN-α, antivirals (e.g. entecavir, tenofovir), maternal prophylaxis
- Hep C: IFN, ribavirin, direct-acting antivirals
- Hep D: No specific treatment, control Hep B
- Hep A/E: Supportive only
- EBV/CMV/HSV: Antivirals (e.g. aciclovir for HSV) if immunocompromised
Complications
- Cirrhosis
- Portal hypertension
- Hepatocellular carcinoma (especially Hep B, C)
- Fulminant liver failure (Hep E in pregnancy, paracetamol overdose)
- Chronic liver disease
- Extrahepatic manifestations: diabetes, arthropathy, encephalopathy
Differential Diagnosis
- Autoimmune hepatitis
- Wilson’s disease
- NAFLD/NASH
- Primary biliary cholangitis
- Drug-induced liver injury
- Sepsis-related cholestasis
Summary
Hepatitis encompasses a broad spectrum of liver inflammation caused by viruses, alcohol, drugs, and infections. Chronic forms, particularly from Hep B and C, are major contributors to cirrhosis and liver cancer. Recognition of viral patterns, toxic risk factors, and appropriate serological testing is essential for diagnosis and management. For a broader understanding of liver pathology, refer to our Gastrointestinal Overview page.