Table of Contents
Overview – Liver Failure and Cirrhosis
Liver failure and cirrhosis represent end-stage hepatic conditions with diverse aetiologies, including viral hepatitis, alcohol misuse, toxins, autoimmune disease, and genetic disorders. Cirrhosis develops as a chronic, fibrosing process in response to sustained liver injury, whereas fulminant hepatic failure is an acute and potentially reversible entity marked by rapid hepatocyte necrosis. Recognising and managing these conditions promptly is critical, as both are major causes of morbidity and mortality worldwide, often requiring liver transplantation as definitive therapy.
Fulminant Hepatic Failure
Definition
Acute and severe liver failure characterised by the sudden onset of hepatic encephalopathy and coagulopathy, typically within 2 weeks of the initial liver insult.
Aetiology
Common causes include:
- Viral hepatitis – Hep A, B, D, E
- Drugs – Paracetamol, halothane, antiepileptics, MDMA (ecstasy)
- Toxins – Amanita mushrooms
- Metabolic – Wilson’s disease
- Autoimmune – Autoimmune hepatitis
Morphology
- Massive, diffuse hepatocellular necrosis throughout the liver parenchyma


Clinical Features
- Symptoms:
- Jaundice
- Vomiting
- Fever
- Rapid development of encephalopathy (within 2 weeks)
- Signs:
- Small, soft liver
- Fetor hepaticus
- Cerebral oedema
Investigations
- FBC – To explore aetiology
- LFTs – ↑ALT/AST, ↑Bilirubin
- Coagulation screen – ↓Prothrombin time, ↓Factor V
- Ultrasound – Liver size, vascular patency
Management
- Treat underlying cause
- Supportive care (e.g. fluids, ICU monitoring)
- Vitamin K, fresh frozen plasma, platelets for coagulopathy
- Liver transplant – Only definitive treatment
Hepatic Cirrhosis
Aetiology
- Toxins – Alcohol, drugs (60–70%)
- Chronic viral hepatitis – HBV, HCV (10%)
- Biliary disease – PBC, obstructive cholangiopathies (10%)
- Genetic/metabolic – Haemochromatosis, Wilson’s disease, α1-antitrypsin deficiency
- Cryptogenic – 5%
- Other rare causes
Pathogenesis
Chronic hepatocyte injury → inflammation and necrosis → nodular fibrosis → architectural distortion and functional failure.
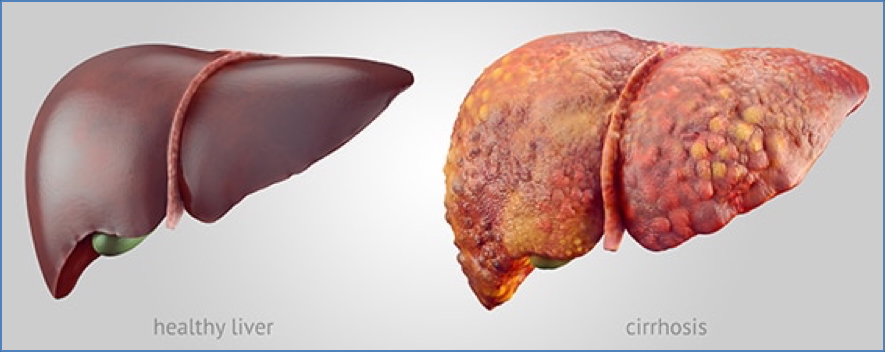
Morphology
- Macro: Shrunken liver, fibrous septa, nodular surface
- Micro: Regenerating nodules surrounded by fibrotic bands
Clinical Features
- Encephalopathy – Confusion, asterixis, coma (↑Ammonia)
- Portal hypertension – Caput medusae, varices, ascites, splenomegaly
- Hormonal dysregulation:
- Spider naevi, palmar erythema
- Gynaecomastia
- Testicular atrophy
Investigations
- ↓Serum albumin
- ↑Prothrombin time
- ↑ALT/AST (esp. if decompensated)
- ↓Na⁺ (hyponatraemia)
- Screen for Wilson’s (serum copper) and α1-antitrypsin deficiency in young patients
Treatment
- Eliminate or treat underlying cause
- Definitive: Liver transplantation
Prognosis
- Irreversible once established
- High mortality without transplant
Signs & Symptoms of Liver Disease
Acute Liver Disease
- Symptoms: Malaise, fever, anorexia (if viral); may be asymptomatic
- Signs: Jaundice or anicteric, hepatomegaly, pale stools, dark urine
Chronic Liver Disease
- Symptoms:
- RUQ pain, pruritus, abdominal distension
- Endocrine symptoms: ↓libido, gynaecomastia, amenorrhoea
- Encephalopathy: confusion, drowsiness
- Signs:
- Jaundice, fever, spider naevi, hepatosplenomegaly
- Ascites, caput medusae, peripheral oedema
- Dupuytren’s contracture, xanthelasmas, testicular atrophy
Hepatic Encephalopathy
- Cause: ↑Ammonia due to impaired hepatic detoxification
- Symptoms: Confusion, irritability, tremor, seizures, coma
- Signs: Asterixis (flapping tremor)
Ascites
- Mechanisms:
- Portal hypertension → ↑hydrostatic pressure
- Hypoalbuminaemia → ↓oncotic pressure
- Hepatorenal syndrome exacerbates volume retention → worsens ascites

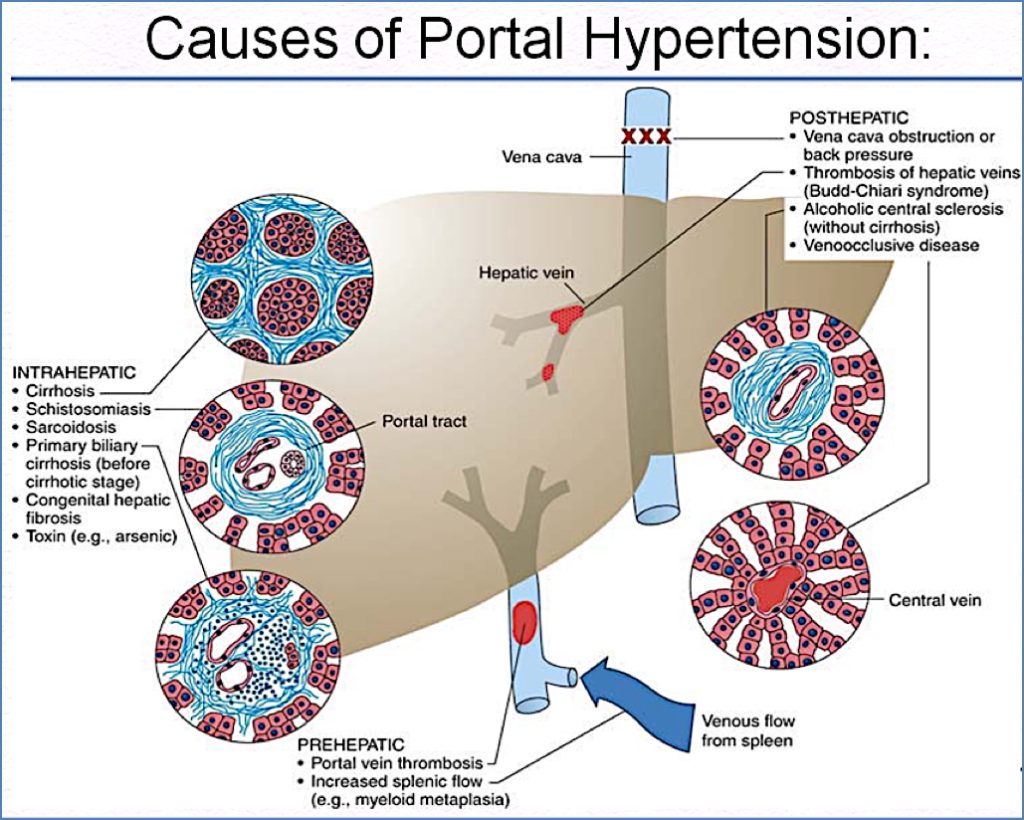
Portal Hypertension
Causes by Level:
- Pre-hepatic: Portal vein thrombosis
- Intra-hepatic: Cirrhosis, schistosomiasis
- Post-hepatic: Hepatic vein thrombosis, Budd-Chiari Syndrome
Summary – Liver Failure and Cirrhosis
Liver failure and cirrhosis are critical hepatic conditions with wide-ranging causes and clinical impacts, from encephalopathy and ascites to portal hypertension and eventual liver transplant. Early recognition of symptoms, investigation into the underlying cause, and timely management are essential. For further hepatology topics, see our Gastrointestinal Overview page.