Table of Contents
Overview – Peptic Ulcer Disease
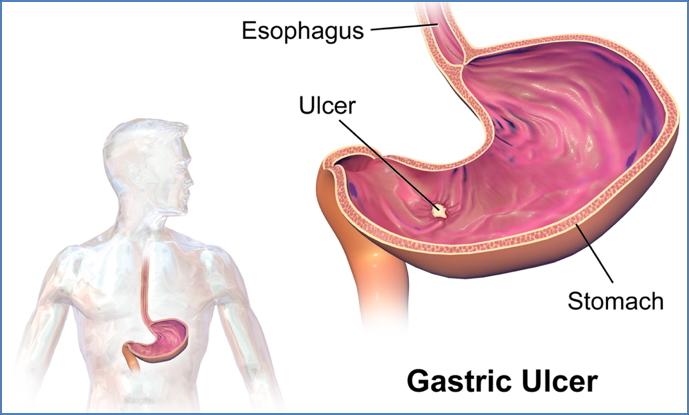
Peptic Ulcer Disease (PUD) is a common and potentially serious gastrointestinal condition characterised by mucosal ulceration, typically in the stomach or proximal duodenum. It arises from an imbalance between protective and destructive gastric factors — most notably due to Helicobacter pylori infection and NSAID use. If untreated, it can lead to bleeding, perforation, and even gastric cancer. Accurate diagnosis and appropriate management are essential to reduce complications and improve patient outcomes.
Protective vs Destructive Factors
Protective Factors
- Alkaline mucus layer → mechanical barrier
- Prostaglandins → stimulate mucin production by goblet cells
Destructive Factors
- Helicobacter pylori
- Gastric acid (pH ~2)
- Pepsin (secreted by chief cells; proteolytic enzyme)
- NSAIDs (e.g. aspirin, ibuprofen)
- Inhibit COX → ↓Prostaglandins → ↓Mucosal protection
- 15–20% of chronic NSAID users develop ulcers
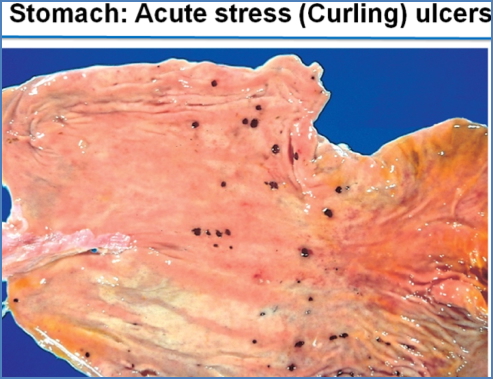
- Stress, especially major burns (Curling’s ulcer)
- Zollinger-Ellison Syndrome (gastrinoma → hyperacidity)
Aetiology
Ulcers arise due to:
- ↑Attack: hyperacidity, Zollinger-Ellison syndrome
- ↓Defence: H. pylori, NSAIDs/corticosteroids, alcohol, smoking, stress
Morphology
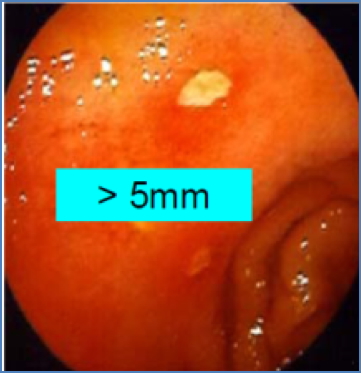
- Typically small, round, single ulcers with sharply punched-out appearance
- Located most commonly in the duodenum or on the lesser curvature of the stomach
- Healing ulcers may show radiating mucosal folds due to scar contraction

2. BruceBlaus, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Clinical Features
- Burning epigastric pain (classically worse on an empty stomach, relieved by food)
- Nausea and vomiting
- Anorexia and weight loss
- Haematemesis or melena (if bleeding)
- Potential signs of complications:
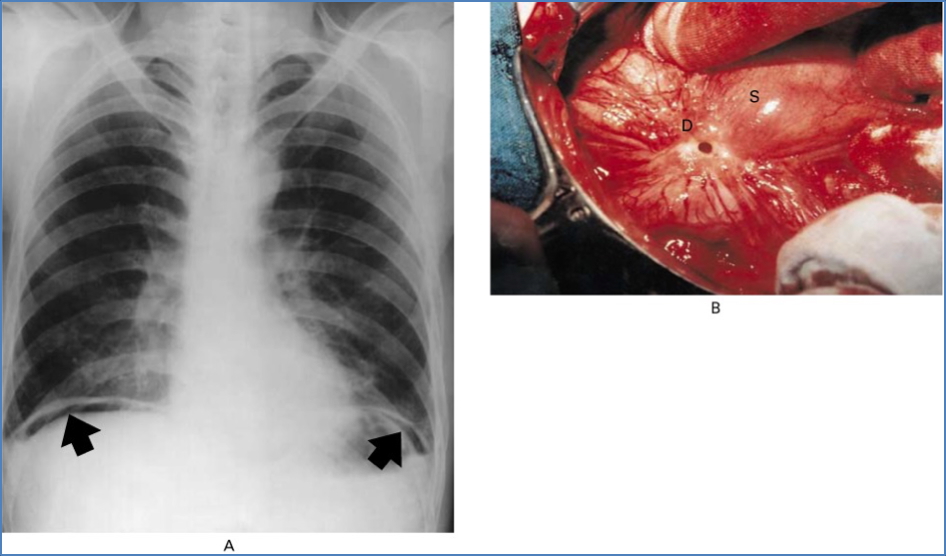
- Perforation → sudden pain, signs of peritonitis
Investigations
- Clinical history
- Endoscopy + Biopsy – assess ulcer, test for H. pylori, rule out gastric cancer
- C13 Urea Breath Test – best non-invasive test for H. pylori
- Serology (IgG antibodies) – H. pylori exposure
- Faecal antigen test – H. pylori detection
Management
Conservative
- Avoid NSAIDs, alcohol, smoking
- Diet modification
Medical
- Antacids (e.g. Mylanta)
- Proton pump inhibitors (e.g. Omeprazole)
- H2-receptor antagonists (e.g. Ranitidine)
- H. pylori eradication:
- Triple therapy: Clarithromycin + Amoxicillin ± Metronidazole
Surgical
- Reserved for complications:
- Haematemesis
- Perforation
- Peritonitis
- Malignancy
Complications
- GI bleeding → anaemia
- Perforation → shock, peritonitis, possible pancreatitis
- Pyloric stenosis (scarring) → gastric outlet obstruction
- Gastric cancer: H. pylori infection increases risk x6
Special Entity – Curling’s Ulcer
Definition
- Acute duodenal ulcer secondary to severe burns and hypovolaemia
Pathogenesis
- ↓Plasma volume → mucosal ischaemia → ulceration
Complications
- High risk of perforation and bleeding
- High mortality if untreated
Prevention & Management
- TPN (total parenteral nutrition)
- PPIs (e.g. Omeprazole) / H2RAs (e.g. Ranitidine)
- Emergency surgery if complications arise
Summary – Peptic Ulcer Disease
Peptic Ulcer Disease results from an imbalance between gastric defence mechanisms and aggressive factors like Helicobacter pylori, NSAIDs, and acid. It typically presents with epigastric pain, and complications include bleeding, perforation, and gastric outlet obstruction. Early diagnosis and eradication of H. pylori are critical. For more, refer to our Gastrointestinal Overview page.