Table of Contents
Overview
Pancreatitis is inflammation of the pancreas that can be acute or chronic. Acute pancreatitis is a medical emergency often triggered by gallstones or alcohol, while chronic pancreatitis involves long-term damage and fibrosis. Complications may include multi-organ failure, diabetes, malabsorption, or pancreatic cancer. Understanding the presentation, causes, complications, and management of pancreatitis is essential for final-year medical students preparing for clinical exams and acute care settings.
Definition
Pancreatitis refers to inflammation of the pancreas, which can be classified as:
- Acute Pancreatitis: Sudden inflammation, often reversible.
- Chronic Pancreatitis: Persistent inflammation with irreversible structural changes and functional loss.
Aetiology
Acute
- Gallstones (50%) – Cholelithiasis → Obstruction of the ampulla or common bile duct
- Alcohol (40%)
- Other causes (10%):
- Infections
- Metabolic (Hypercalcaemia, DKA, uraemia)
- Trauma
- Ischaemia
- Duodenal ulcer
- Drugs
- Scorpion venom
- Idiopathic
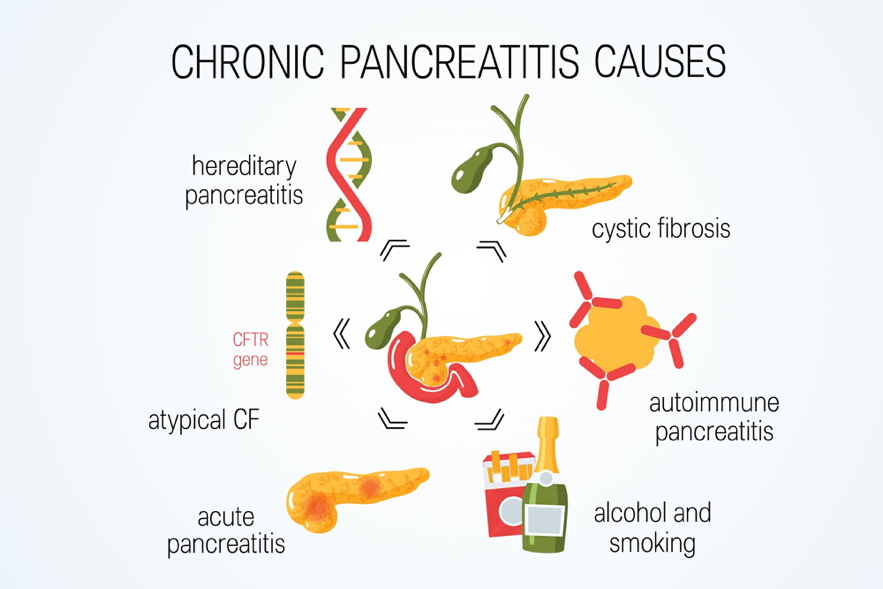
Chronic
- Alcohol abuse (most common)
- Biliary tract disease
- Hypercalcaemia
- Pancreatic divisum
- Familial pancreatitis
- Cystic fibrosis
Pathogenesis
Acute
- Autodigestion of the pancreas by its own enzymes → Inflammation ± necrosis
- Can trigger Systemic Inflammatory Response Syndrome (SIRS):
- Shock
- Acute renal failure
- ARDS (Acute Respiratory Distress Syndrome)
Chronic
- Recurrent inflammation → Exocrine atrophy and fibrosis
- Progressive ductal obstruction → irreversible pancreatic damage
Clinical Features
Acute
- Acute abdominal emergency
- Symptoms:
- Epigastric/upper abdominal pain (often post-meal or alcohol-triggered)
- Vomiting
- Guarding, rigidity (peritonitis)
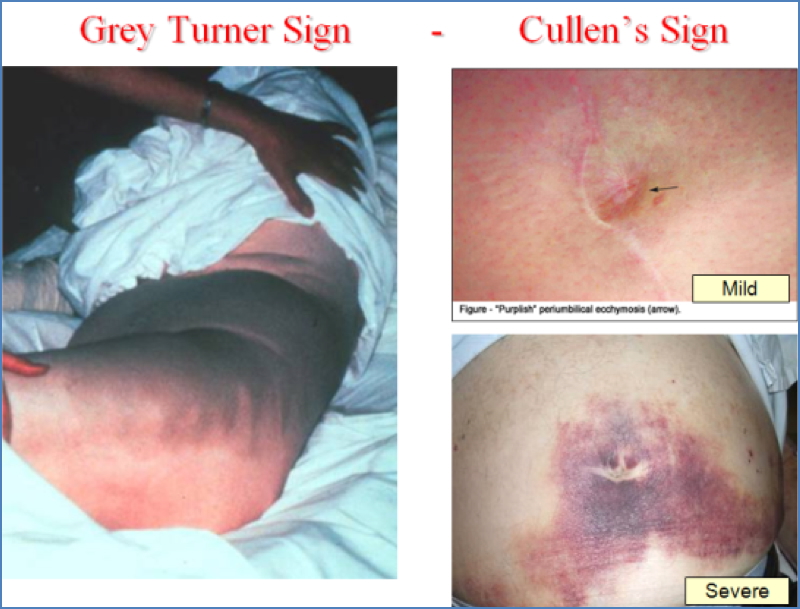
- Haemorrhagic signs:
- Grey Turner’s sign (flank bruising)
- Cullen’s sign (periumbilical bruising)
- Local complications:
- Pancreatic abscess
- Infected necrosis
- Pseudocysts
- Duodenal obstruction
- Systemic complications:
- Jaundice
- DIC
- ARDS
- Acute renal failure
Chronic
- Symptoms:
- Recurrent abdominal pain
- Steatorrhoea
- Weight loss
- Jaundice
- Secondary diabetes mellitus
- Complications:
- Progressive exocrine and endocrine failure
- Pseudocyst formation
- Biliary duct obstruction
- Risk of pancreatic carcinoma
Investigations
- Rule out other causes of acute abdomen:
- Appendicitis, diverticulitis, peptic ulcer, cholecystitis, bowel obstruction, ischaemia
- Serum amylase – rises within 24 hours (sensitive)
- Serum lipase – more specific; rises after 72 hours
- FBC – neutrophilic leukocytosis
- LFTs – raised ALP and bilirubin (if biliary obstruction)
- Imaging:
- Ultrasound/CT/MRCP
- ERCP in biliary or obstructive cases
- Biopsy is contraindicated in acute cases due to risk of exacerbation
Management
Acute
- Supportive care:
- NBM
- IV fluids and electrolyte correction
- Analgesia
- Severe cases:
- ICU admission
- Prophylactic antibiotics (if necrosis)
- Rarely surgical intervention
Chronic
- Supportive care:
- Pain control, hydration, nutrition
- If endocrine/exocrine failure:
- Creon Forte (enzyme replacement)
- Insulin (for secondary diabetes)
- Manage associated biliary pathology
- Address lifestyle factors (especially alcohol)
Prognosis
- Acute:
- 80% recover with supportive care
- 20% develop severe, life-threatening complications
- Chronic:
- Progressive loss of pancreatic function
- Requires lifelong medical management and monitoring
Summary
Pancreatitis is an inflammatory condition of the pancreas that can be acute or chronic. Acute pancreatitis is usually caused by gallstones or alcohol and can lead to life-threatening systemic complications. Chronic pancreatitis results from recurrent inflammation leading to fibrosis, pancreatic insufficiency, and increased cancer risk. For more detail, explore our Gastrointestinal Overview page.