Table of Contents
Overview – Polyps & Colon Cancer
Polyps and colon cancer form a spectrum of colonic neoplasia, ranging from benign mucosal outgrowths to highly invasive adenocarcinomas. Colorectal cancer (CRC) is the second most common internal malignancy and a leading cause of cancer-related death in developed countries. Early identification and polypectomy can be curative, underscoring the importance of screening programs. This article reviews the different types of colonic polyps, risk factors, pathogenesis, clinical presentation, and management of colorectal cancer.
Definition
- Colonic Polyps: Mucosal outgrowths in the colon; may be non-neoplastic or neoplastic (precancerous).
- Colorectal Cancer (CRC): Adenocarcinoma arising from colonic epithelium, often through the adenoma–carcinoma sequence.
Aetiology
Risk Factors
- Age >50 (90% of CRC diagnosed in older adults)
- Pre-existing adenomatous polyps
- Family history – HNPCC (Lynch syndrome), FAP
- IBD – Crohn’s disease, Ulcerative colitis
- Diet – High-fat, low-fibre, low-calcium, low-folate
- Smoking
Pathophysiology
- Mutation (sporadic or inherited) → cell cycle dysregulation → dysplasia → adenoma → carcinoma
- >95% sporadic (typically left-sided/distal colon)
- <5% inherited (typically right-sided/proximal colon)
Morphology
- 98% of colonic neoplasms are adenocarcinomas
- May arise from benign polyps, particularly adenomas
Clinical Features
- Often asymptomatic early
- Altered bowel habit (constipation, diarrhoea, or both)
- Thin, ribbon-like stools
- Cramping abdominal pain, bloating
- Rectal bleeding – detected via Faecal Occult Blood Test (FOBT)
- Left-sided (sporadic): frank bleeding
- Right-sided (familial): occult bleeding → anaemia
- Red flags: anorexia, fever, night sweats, weight loss, fatigue, iron-deficiency anaemia
Investigations
- FOBT (screening)
- Colonoscopy – gold standard for diagnosis/polypectomy/biopsy
- CT / PET / Barium enema – staging and localisation
- Genetic testing – if family history suspicious
- FBC – for anaemia
Types of Polyps
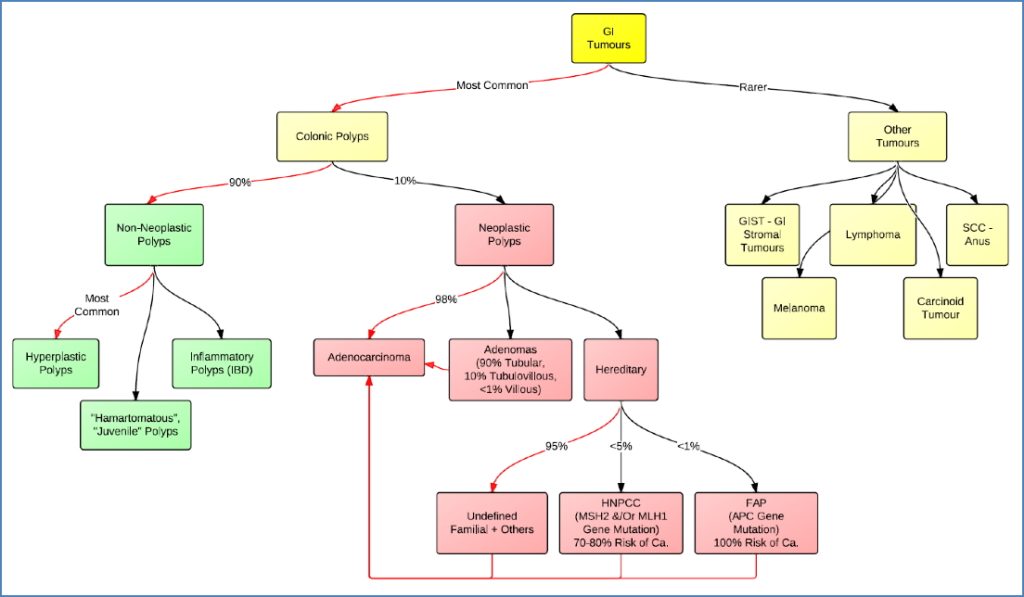
Non-Neoplastic (90%)
- Hyperplastic Polyps
- Most common; small, sessile; no dysplasia
- “Saw-tooth” histology; increased goblet cells
- Distal colon

- Hamartomatous / Juvenile Polyps
- Benign malformations, common in Peutz-Jeghers syndrome
- May obstruct

- Inflammatory (Pseudopolyps)
- Associated with IBD

Neoplastic (10%)
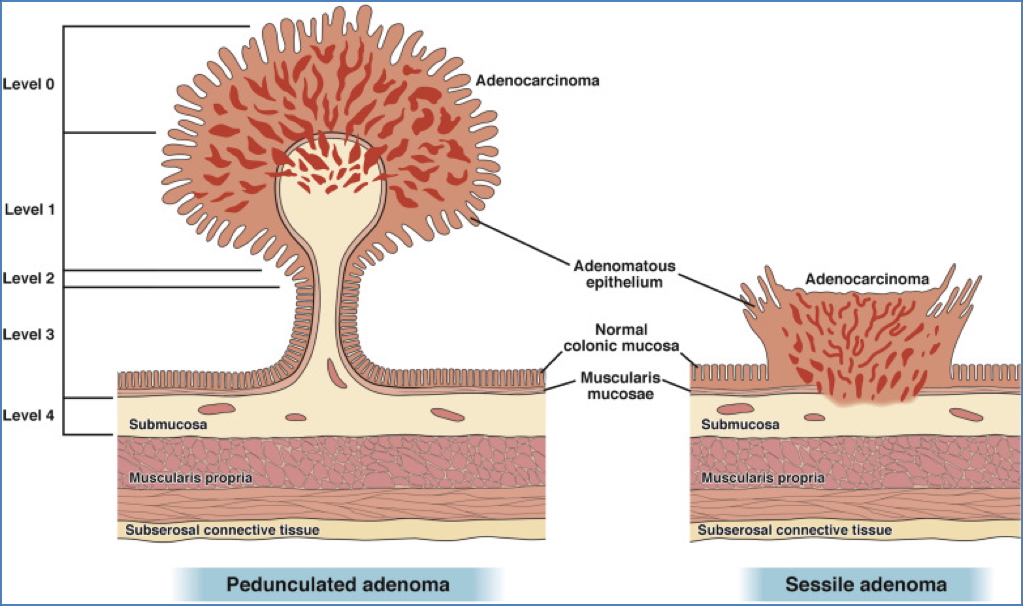
- Adenomas
- Tubular (90%) – pedunculated
- Tubulovillous (<10%) – mixed pattern
- Villous (<1%) – sessile, highest malignancy risk
Types of Colorectal Cancer
Adenocarcinoma (98%)
- Sporadic or inherited
- ↑ Incidence in Western populations and elderly
- May begin as adenoma → carcinoma sequence

Hereditary Non-Polyposis Colon Cancer (HNPCC / Lynch Syndrome)
- Autosomal dominant; 70–80% lifetime CRC risk
- Few polyps, but high transformation risk
- ↑ Risk of other cancers: endometrial, ovarian, gastric, renal
- Amsterdam II Criteria:
- ≥3 affected relatives
- One must be a 1st-degree relative
- Involvement across ≥2 generations
- At least one case <50yo

Familial Adenomatous Polyposis (FAP)
- Autosomal dominant; thousands of adenomas
- 100% cancer risk if untreated
- Also increases risk for other GI and extra-GI cancers
- Requires prophylactic colectomy

Management
- Colonoscopy + Polypectomy (for diagnosis and prevention)
- Staging: CT / PET / MRI; TNM or Duke’s classification
- Definitive treatment:
- Surgical resection ± colostomy
- Targeted biologics (e.g. Cetuximab, Panitumumab)
- Chemotherapy ± Radiotherapy

Complications
- Perforation, abscess, or fistula
- Peritonitis
- Metastasis → death
Summary – Polyps & Colon Cancer
Polyps and colon cancer represent a continuum from benign lesions to malignant neoplasia. Most polyps are non-neoplastic and carry low risk, but adenomas can transform into colorectal cancer if left untreated. Early detection through FOBT and colonoscopy is key. Inherited syndromes like FAP and HNPCC require targeted surveillance and sometimes prophylactic surgery. For further context, see our Gastrointestinal Overview page.