Table of Contents
Overview – Rectal Bleeding
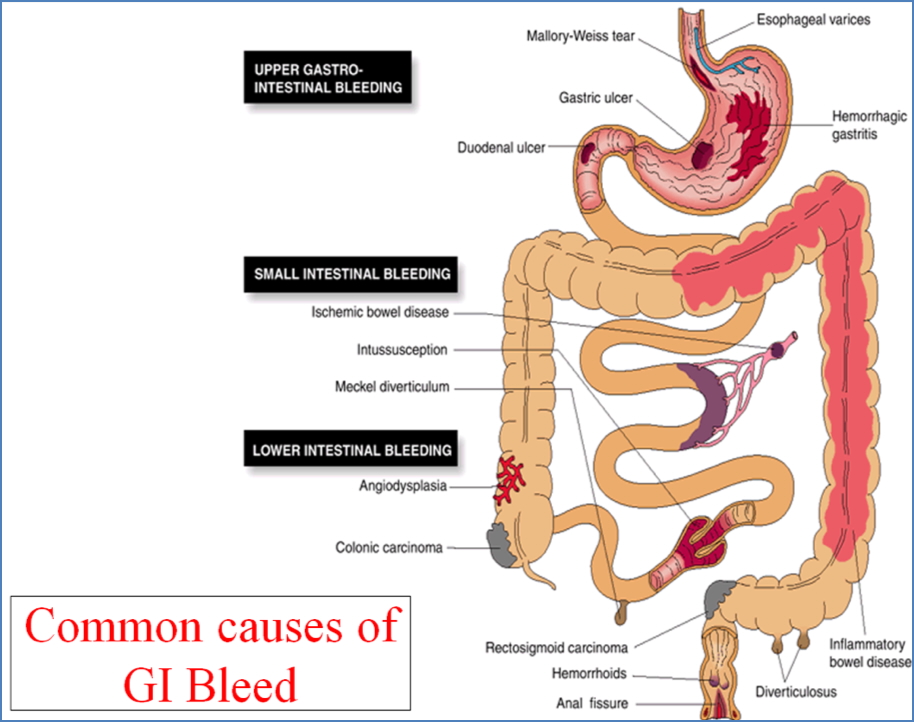
Rectal bleeding is a common but potentially serious clinical symptom, often prompting urgent assessment in both primary care and emergency settings. It may range from benign anorectal causes like haemorrhoids to life-threatening upper gastrointestinal haemorrhage. Accurate identification of the source — upper versus lower GI tract — is essential for effective triage and management. This page provides a high-yield approach to the differential diagnosis, investigations, and management strategies for rectal bleeding, tailored for final-year medical students.
Definition
Rectal bleeding refers to the passage of blood through the anus. It may be visible to the patient (gross bleeding) or occult (hidden and detected via testing). It can be painless or painful, and may originate from any part of the gastrointestinal tract.
Terminology
- Haematemesis
- Vomiting of blood (fresh or denatured/coffee-ground)
- Suggests bleeding from the stomach or oesophagus
- Emergency — requires rapid IV access and cross-matching
- Haematochezia
- Passage of bright red or maroon blood per rectum
- Major bleeding → Often upper GI
- Minor bleeding → More likely lower GI
- Melaena
- Black, tarry stool from digested blood
- Typically implies upper GI bleeding
- Occult Bleeding
- Not visible to the naked eye
- Often discovered via faecal occult blood test (FOBT)
- May present as iron-deficiency anaemia
Major Rectal Bleeding
Defined as bleeding that results in haemodynamic instability and requires resuscitation (e.g. tachycardia, hypotension, pallor, altered level of consciousness).
Common Causes – Upper GI:
- Peptic ulcer disease
- Duodenal ulcers
- Oesophageal varices
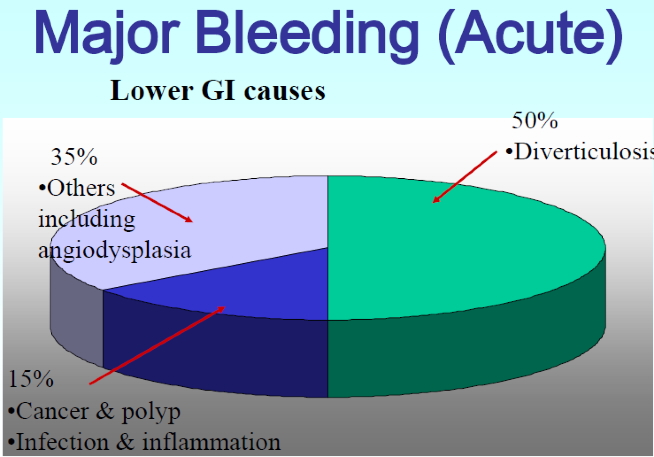
Common Causes – Lower GI:
- Diverticulosis (~50%)
- Angiodysplasia (~35%)
- Colorectal cancer (~15%)
TIP:
- Bright red (frank) blood → Suggests distal or brisk bleeding
- Dark/black blood → Slower bleed or more proximal origin
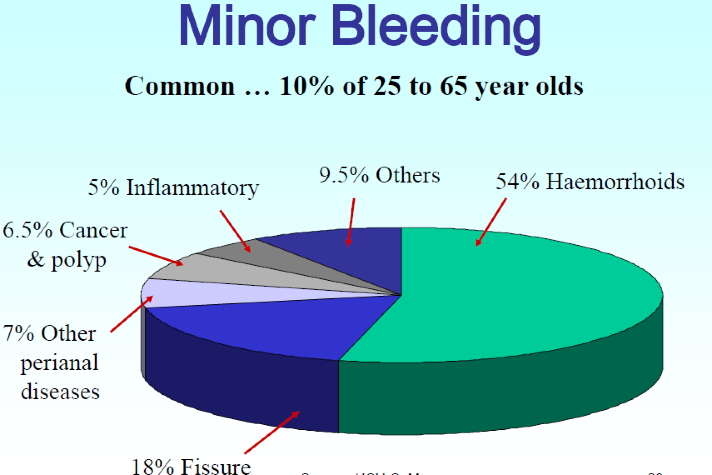
Minor Rectal Bleeding
Occurs in haemodynamically stable patients and often results from benign anorectal pathology.
Common Causes – Lower GI:
- Haemorrhoids (~54%)
- Anal fissure (~18%)
- Fistulae (~7%)
- Colorectal polyps or cancer (~6%)
Investigations
- FBC: Assess for anaemia, reticulocytosis, thrombocytopenia
- Coagulation panel: PT, INR, APTT
- LFTs: To assess for liver disease (especially if varices suspected)
- EUCs: Fluid status and renal function
- FOBT: To detect occult bleeding
- Endoscopy / Colonoscopy: Gold standard for localisation and diagnosis
Management
- Initial Stabilisation:
- Large-bore IV access
- Intravenous fluid resuscitation
- Group & Hold and cross-match for transfusion if severe
- Pharmacological Measures:
- PPI if peptic ulcer disease suspected
- Definitive Treatment:
- Endoscopy or colonoscopy ± therapeutic intervention

Summary – Rectal Bleeding
Rectal bleeding is a high-yield clinical presentation that can signal anything from benign haemorrhoids to significant gastrointestinal pathology. Differentiating upper vs lower GI sources and identifying major vs minor bleeding are crucial steps in early management. Prompt investigation and stabilisation can prevent complications and guide definitive therapy. For a broader context, see our Gastrointestinal Overview page.