Table of Contents
Overview – Hypersensitivity & Allergy
Hypersensitivity & allergy refer to abnormal, often exaggerated immune responses that cause harm to the host. These reactions may be triggered by harmless environmental antigens or the body’s own tissues. They form the basis of many allergic, autoimmune, and drug-induced conditions commonly encountered in clinical medicine. Understanding the mechanisms and types of hypersensitivity is essential for recognising, diagnosing, and treating diseases such as asthma, anaphylaxis, contact dermatitis, and serum sickness.
Definition
- Hypersensitivity = An abnormal immune reactivity that leads to tissue damage or systemic disease.
- Often triggered by innocuous antigens such as pollen or food.
- Atopy = Genetic tendency to produce immediate hypersensitivity (usually IgE-mediated) to common environmental antigens.
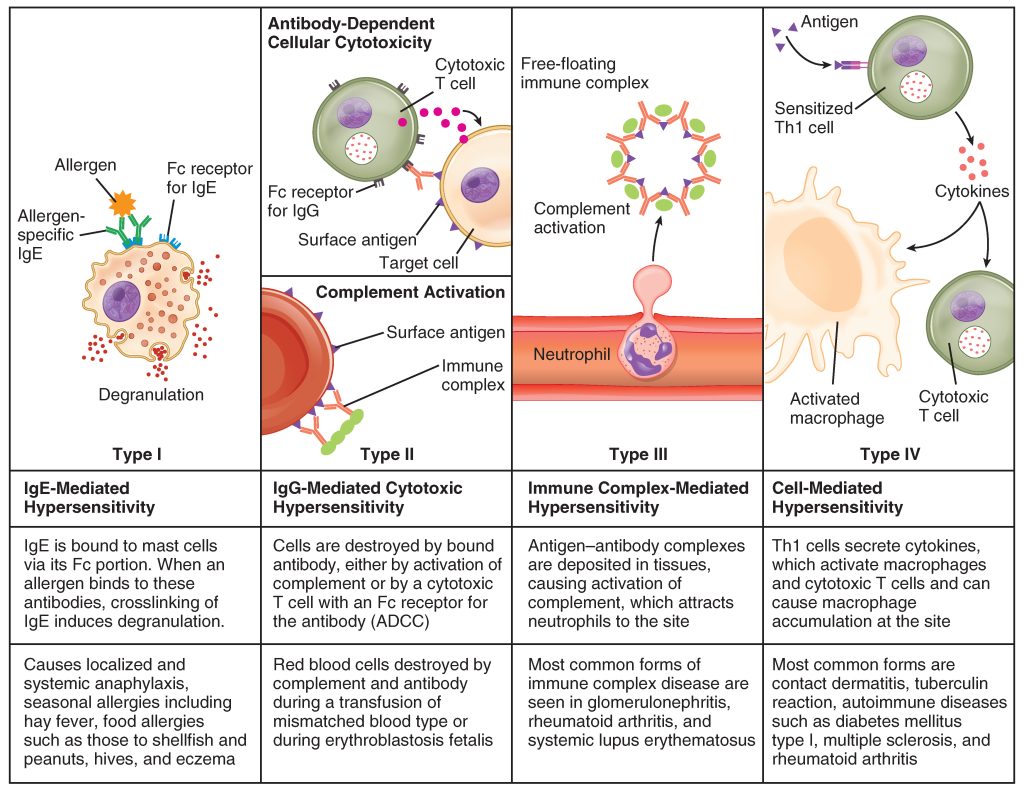
Classification of Hypersensitivity
There are 4 recognised types of hypersensitivity:
- Type I – Anaphylactic (IgE-mediated)
- Type II – Antibody-dependent cytotoxicity
- Type III – Immune complex-mediated
- Type IV – Cell-mediated (T cell)
Types I–III involve B cell/antibody-mediated responses; Type IV is a T cell-mediated phenomenon.

Type I Hypersensitivity – IgE-Mediated (Anaphylaxis, Allergy)
Pathophysiology
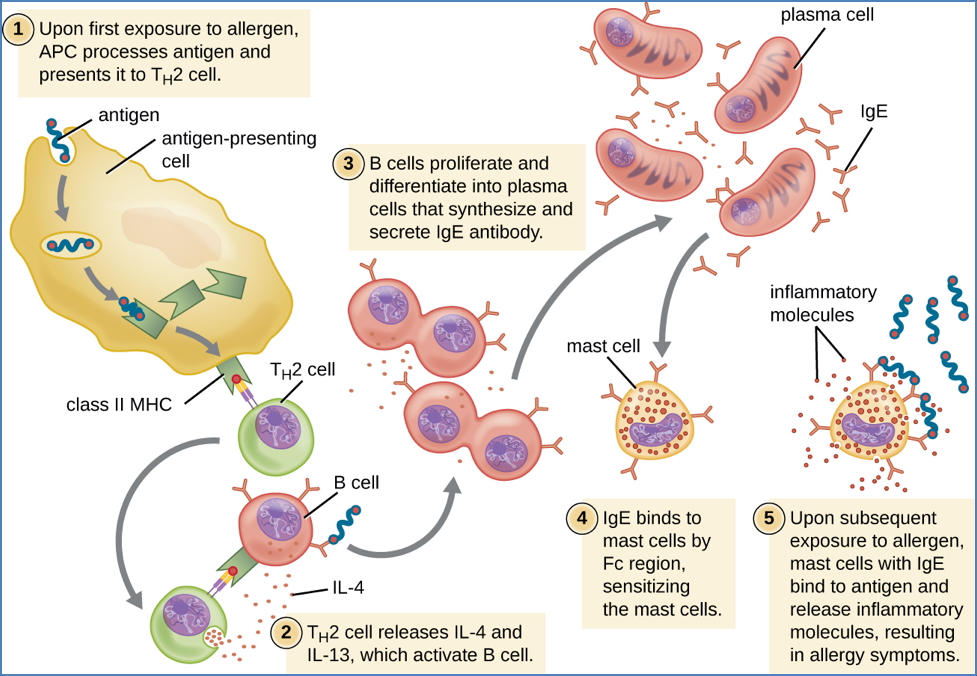
- Mediated by Th2 cells, IgE antibodies, and mast cells
- Initial allergen exposure → APCs (antigen-presenting cells) activate Th2 cells
- Th2 cells secrete IL-4 and IL-13 → Activate B cells → Class switch to IgE
- IgE binds Fcε receptors on mast cells → Sensitisation phase
- Re-exposure to allergen → Cross-linking of bound IgE → Mast cell degranulation
- Release of inflammatory mediators:
- Histamine → Vasodilation, ↑vascular permeability, bronchospasm
- Leukotrienes, prostaglandins → Mucus secretion, smooth muscle contraction
- IL-4, TNFα, CCL3 → Potentiation of inflammation and recruitment of phagocytes
Bi-Phasic Response
- Immediate Phase (seconds–minutes): Preformed mediators (histamine, PGs)
- Late Phase (8–12 hours): Synthesised mediators (cytokines, leukotrienes, chemokines) → oedema
Clinical Examples
- Allergic Asthma
- Triggered by allergens, viruses, smoke, cold air, NSAIDs
- Bronchoconstriction → Wheeze, hyperinflation, airflow limitation
- Late-phase = airway remodelling (↑SM, oedema, mucus)
- Diagnosis: Spirometry (obstructive), elevated IgE
- Management: β-agonists (e.g. salbutamol), inhaled corticosteroids
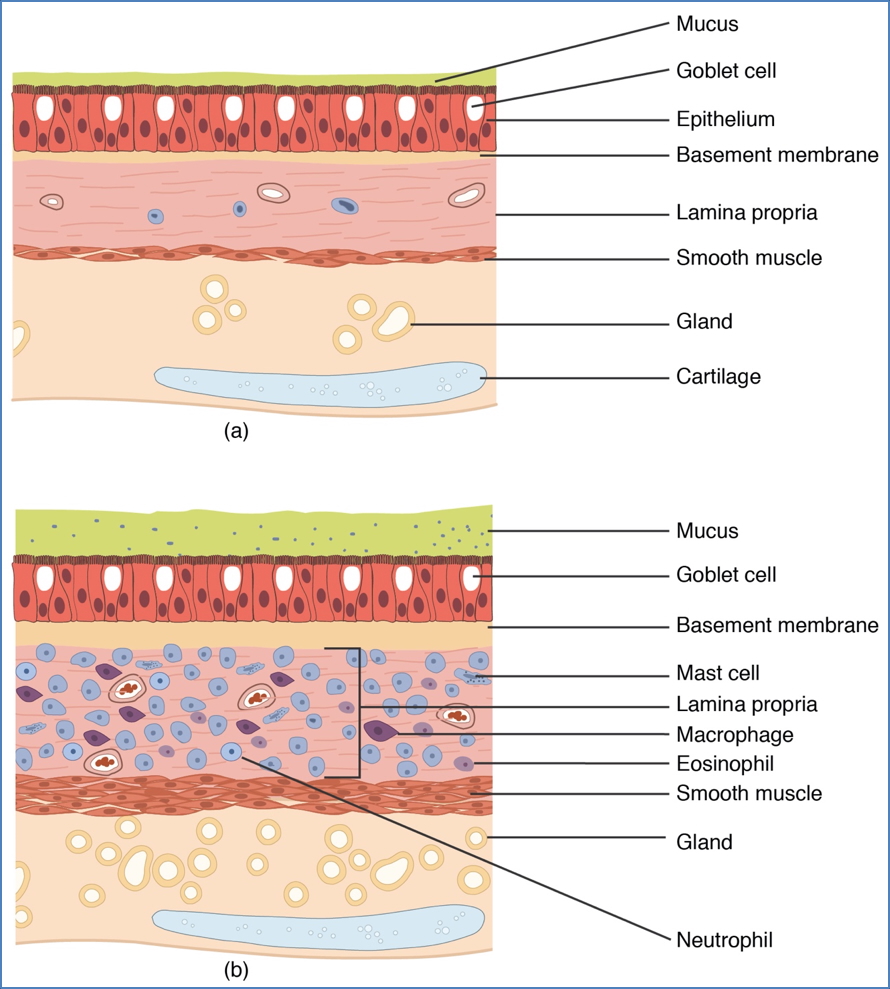
CNX OpenStax, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons
- Allergic Bronchopulmonary Aspergillosis (ABPA)
- Type I reaction to Aspergillus fungus
- Asthma, mucus plugging, IgE↑, eosinophilia, bronchiectasis
- Diagnosis: Skin prick test, IgE to Aspergillus, CXR
- Treatment: Oral corticosteroids (e.g. prednisolone), inhaled corticosteroids
- Allergic Rhinitis
- Sneezing, nasal congestion, rhinorrhoea
- Management: Allergen avoidance, antihistamines, immunotherapy
- Anaphylaxis
- Systemic mast cell degranulation → Widespread vasodilation, oedema, hypotension
- Signs: ↓BP, cold extremities, ↓cerebral/renal/coronary perfusion
- Treatment: Adrenaline, volume resuscitation, remove allergen
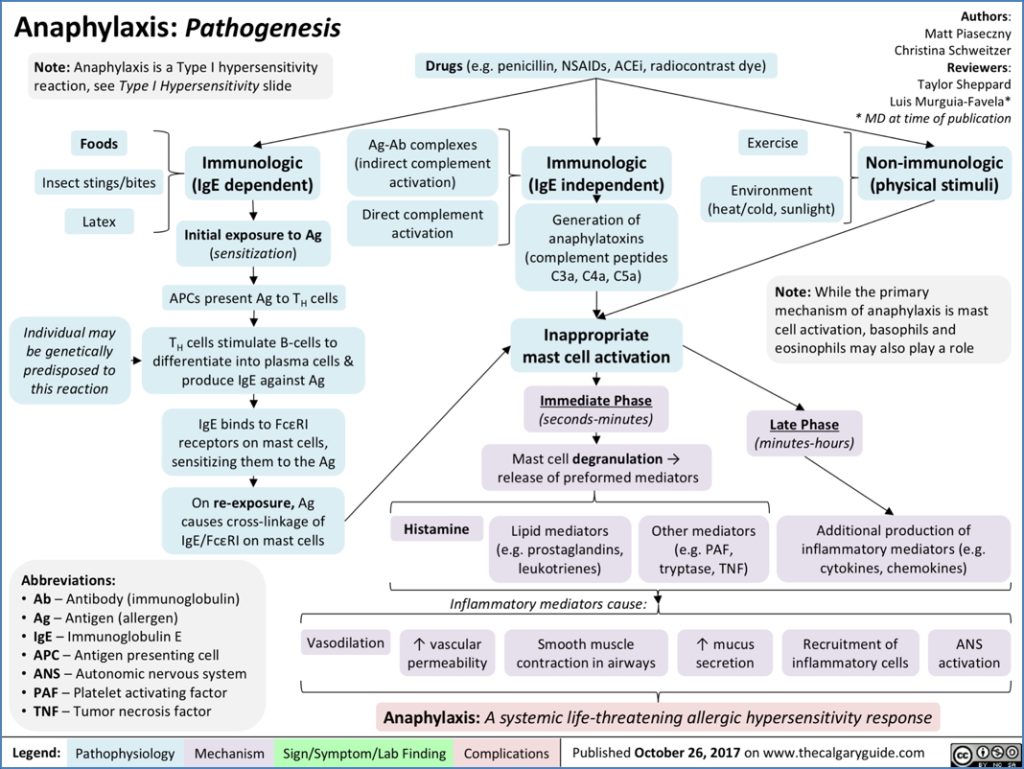
Penicillin-Induced Anaphylaxis
- Penicillin binds to self-proteins → Becomes antigenic
- APCs present modified peptides to Th2 cells → IgE production
- IgE binds mast cells → Re-exposure causes degranulation → Systemic anaphylaxis
Risk Factors & Susceptibility
- Genetic: Atopy is familial; varies by ethnicity
- Environmental:
- Hygiene Hypothesis – Low early microbe exposure → ↑atopy
- Allergen levels, pollution, dietary changes

Immunological Basis for Hypo-Sensitisation
- Allergen immunotherapy: Gradual allergen exposure aims to shift Th2 → Th1 response
- ↓IgE production → ↓mast cell activation → ↓allergy
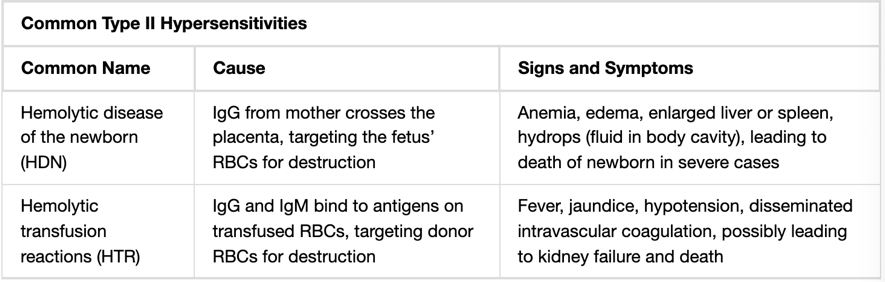
Type II Hypersensitivity – Cytotoxic Antibody-Mediated
Pathophysiology
- IgG binds to host cell surface antigens
- Activates complement or Fc-receptor mediated clearance
- Opsonisation → Phagocytosis/destruction by macrophages
- Tissues or blood cells may be targeted
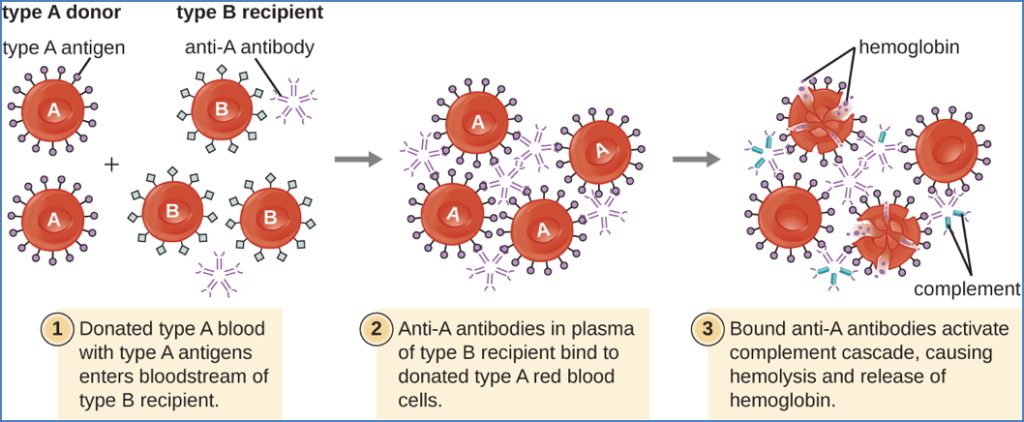
Clinical Examples
- Drug-Induced Haemolytic Anaemia – Anti-drug IgG binds drug-coated RBCs → Splenic clearance
- Autoimmune Thrombocytopenia – Same mechanism on platelets
- Rheumatic Heart Disease – Cross-reaction of anti-M protein antibodies with cardiac tissue
- Transfusion Reactions
Type III Hypersensitivity – Immune Complex-Mediated
Pathophysiology
- Formation and deposition of small Ag-IgG immune complexes
- Triggers complement activation → Inflammation
- Fc-mediated mast cell degranulation → Vasodilation, vascular leakage
- Granulocytes recruited → Tissue injury
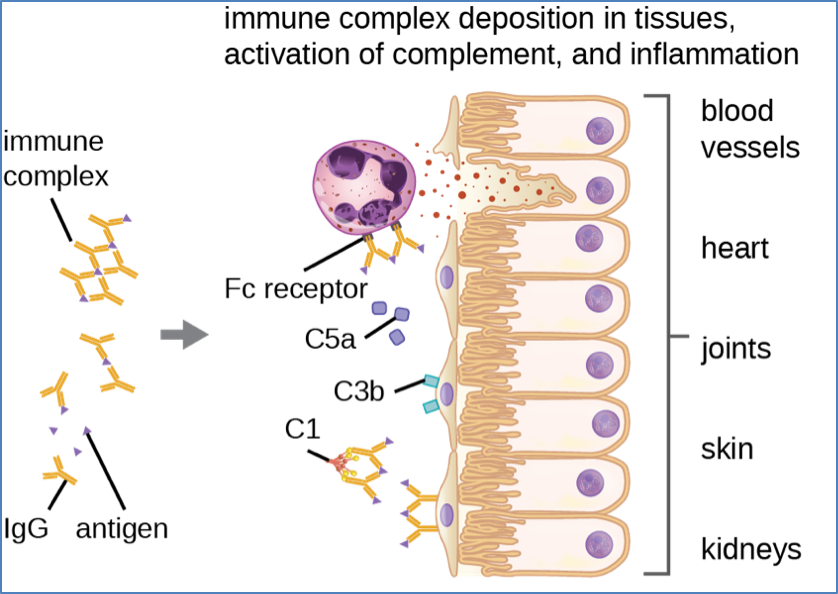
Clinical Examples
- Arthus Reaction – Local vasculitis from intradermal antigen
- Serum Sickness – Systemic vasculitis, arthritis, GN after IV foreign antigen
- Rheumatoid Arthritis – Immune complexes in joints
Type IV Hypersensitivity – T Cell-Mediated (Delayed)
Pathophysiology
- Th1 cells recognise antigen-MHC II complexes on macrophages
- Secrete IFN-γ, TNF-β → Macrophage activation, endothelial activation
- Tissue damage, granuloma formation
- Cytotoxic T cells (CTLs) also cause direct cell killing

Clinical Examples
- Contact Dermatitis – (Th1 mediated)
- Tuberculin Reaction (Mantoux test) – Diagnostic for TB exposure
- Type 1 Diabetes Mellitus – Cytotoxic destruction of β-cells
- Multiple Sclerosis, Coeliac Disease
Summary – Hypersensitivity & Allergy
Hypersensitivity & allergy describe immune responses that result in tissue damage due to misdirected reactivity to foreign or self-antigens. The four types—ranging from IgE-mediated allergy (Type I) to T cell-driven delayed responses (Type IV)—each have distinct mechanisms and clinical consequences. Anaphylaxis, asthma, autoimmune cytotoxicity, and contact dermatitis are just a few key examples. For a broader context, see our Immune & Rheumatology Overview page.