Table of Contents
Overview – Pandemics
Pandemics are large-scale outbreaks of infectious diseases that spread across countries or continents. According to the World Health Organization (WHO), a disease must be novel, cause serious illness in humans, and spread efficiently between people to be classified as a pandemic. This page outlines pandemic definitions, response strategies, resource allocation, and public health ethics—knowledge essential for final-year medical students involved in public health planning.
Definition
WHO Criteria for a Pandemic:
A disease is considered a pandemic when it meets all three of the following criteria:
- Novel: No pre-existing immunity in humans
- Causes serious illness
- Spreads efficiently between humans
Note: A condition like cancer is not a pandemic—even if widespread or fatal—because it is not infectious.
Seasonal influenza is also excluded, as it is not a novel disease.
Pandemic Phases and Management
Pandemic response evolves through distinct phases:
1. ALERT
- Novel zoonotic virus causes severe disease in humans
- No human-to-human transmission yet
- Virus has not reached the home country
2. DELAY
- Virus still outside home country
- OS4: Small overseas clusters
- OS5: Larger clusters in one or two countries
- OS6: Spread to multiple countries
3. CONTAIN
- Virus enters home country
- Small number of local cases detected
4. SUSTAIN
- Community transmission established in the home country
5. CONTROL
- Vaccines available
- Widespread immunisation begins to reduce spread
6. RECOVER
- Pandemic under control domestically
- Ongoing risk of new waves from viral mutations or re-importation
Who Gets Treated?
- Early phases: Treat all cases to reduce transmission
- Later phases: Prioritise at-risk groups due to limited resources
- Financial cost increases significantly when treating the whole population
Vaccine Prophylaxis
Available from the Control phase onwards.
Priority Groups:
- High-risk individuals (e.g. elderly, chronic illness)
- Residents in closed institutions (e.g. prisons, nursing homes)
- Healthcare and essential workers
Vaccine Types:
- Inactivated vaccines – contain killed virus strains
- Subunit vaccines – minimise unnecessary protein components
- Live attenuated vaccines – may be delivered nasally for mucosal immunity
- Recombinant vaccines – produced using DNA technologies
Ethical Allocation of Resources
Key question: Who gets access when resources are scarce?
Ethical Considerations:
- Equal access: Lottery or first-come basis (blind justice)
- Prioritising high-risk individuals
- Protecting healthcare and essential service workers
- Children and vulnerable populations
- Global equity in resource distribution
Example – COVID-19:
- Limited ICU and ED capacity led to:
- Postponing elective surgeries
- Field hospitals to increase bed capacity
Countermeasures in a Pandemic
1. Therapeutic Countermeasures:
- Stockpiling medications and vaccines
- Ensuring access to care and staffing
2. Non-Therapeutic Countermeasures:
- Infection control
- Surveillance and contact tracing
- Social distancing and quarantine
- Travel restrictions and border closures
Isolation and Quarantine
- Isolation: Separates infected individuals for the duration of infectiousness
- Quarantine: Restricts movement of exposed but not yet symptomatic individuals during the incubation period

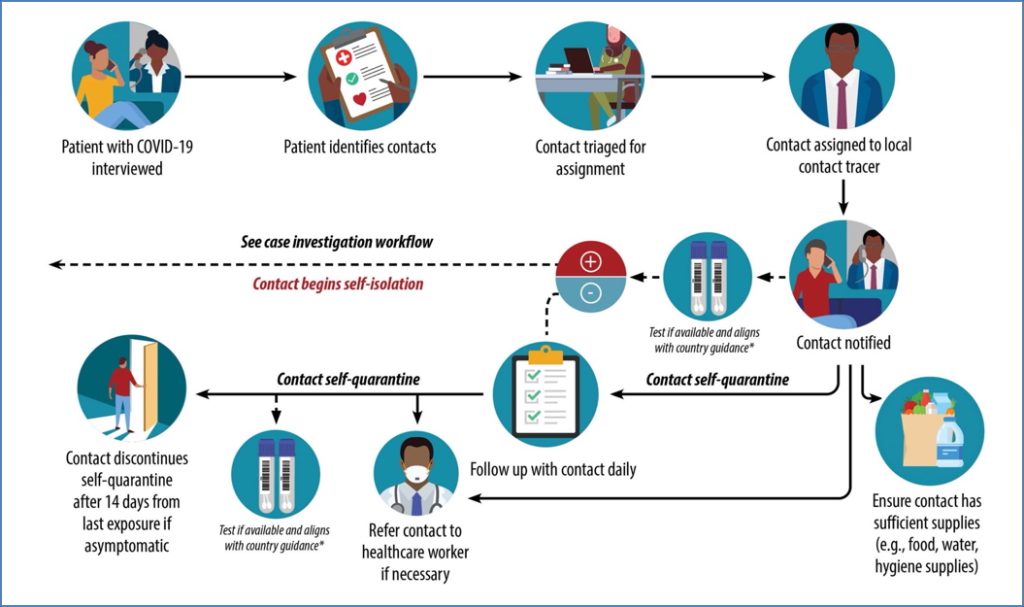
Surveillance and Contact Tracing
- Contact tracing: Identifies and follows up with people who had close contact with a confirmed case
- Surveillance: Includes health declarations, temperature logs, daily monitoring forms
Public Health vs Clinical Ethics
- Clinical Medicine:
- Patient-centred
- Emphasises autonomy, liberty, and best individual outcomes
- Public Health:
- Population-centred
- May override individual freedoms for greater societal benefit
- Examples: quarantine, isolation, lockdowns, border closures
Summary – Pandemics
This pandemics guide outlines the definition, phases of management, vaccine strategies, and ethical dilemmas faced during widespread outbreaks. Understanding public health planning and response is essential for future clinicians navigating population-wide infectious threats. For a broader context, see our Microbiology & Public Health Overview page.