Table of Contents
Overview – Ankylosing Spondylitis
Ankylosing spondylitis is a chronic inflammatory disease primarily affecting the axial skeleton, particularly the sacroiliac joints and spine. It leads to progressive stiffness, pain, and eventual fusion of vertebrae, causing marked postural changes such as kyphosis. This condition typically affects young males and has a strong genetic link with HLA-B27 positivity. Early recognition and targeted treatment are critical to reduce long-term morbidity and improve quality of life. This page will cover the definition, pathophysiology, clinical features, diagnosis, and management of ankylosing spondylitis.
Definition
Ankylosing spondylitis (AS) is a seronegative spondyloarthropathy characterised by chronic inflammation of the axial skeleton, especially the sacroiliac joints and spine, with eventual ossification and fusion (ankylosis) of spinal elements.
Aetiology
- Genetic predisposition
- Strongly associated with HLA-B27
- 100% concordance in monozygotic twins
Pathophysiology
- Inflammation begins at entheses (sites where ligaments/tendons attach to bone)
- In the spine:
- Enthesitis leads to erosion of bone
- Followed by ossification of the annulus fibrosus
- Results in syndesmophyte formation → vertebral fusion → bamboo spine
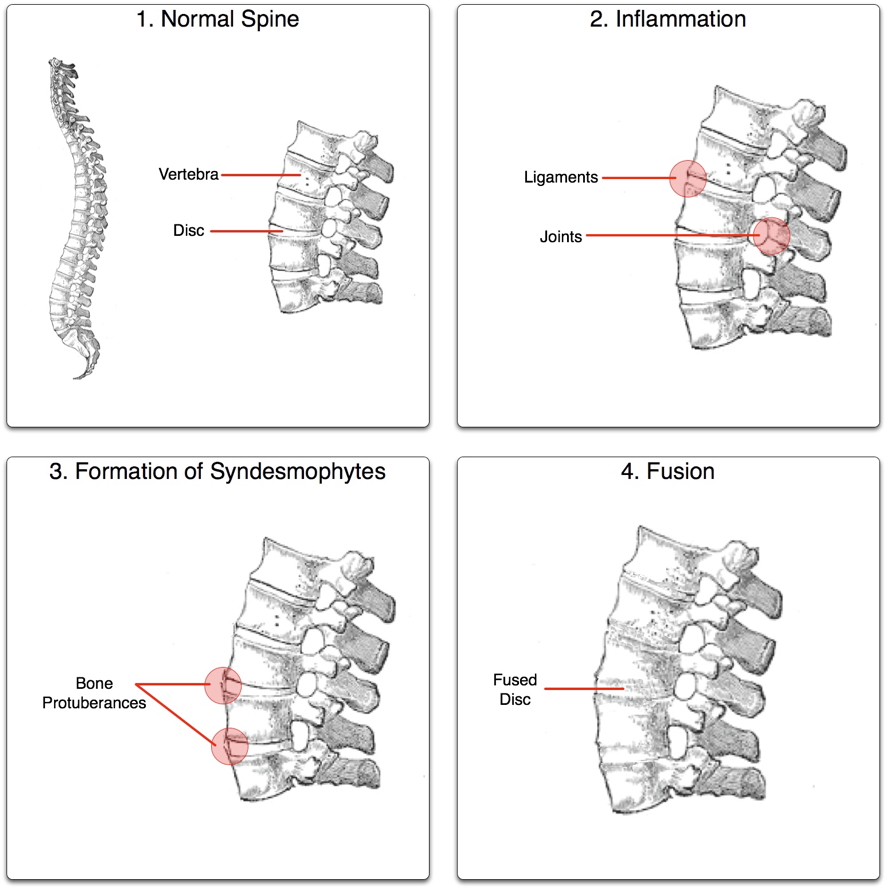
Morphology
- Syndesmophytes: Vertical bony outgrowths bridging vertebrae
- Ankylosis: Fusion of joints, reducing mobility
- Squaring of vertebral bodies: Due to erosion and reactive sclerosis
Clinical Features
Demographics
- Common in males aged 15–25
- Male:Female ratio ~3:1
Axial Involvement
- Lower back pain and morning stiffness
- Sacroiliitis: Persistent buttock pain
- Kyphosis and altered spinal posture
- ↓ Chest wall expansion (restrictive pattern)
Appendicular Involvement
- Asymmetric large joint arthritis (hips, shoulders)
Extra-Articular Features
- Ocular: Iritis, anterior uveitis
- Cardiac: Aortitis, aortic regurgitation, pericarditis
- Renal: IgA nephropathy, amyloidosis
Investigations
Clinical Examination
- ↑ Occiput-to-wall distance
- ↓ Spinal range of motion
- ↓ Chest expansion
- Positive FABER test (sacroiliac joint tenderness)
Imaging
- X-Ray of Sacroiliac Joint:
- Pseudowidening → sclerosis → fusion
- Spinal X-Ray:
- Squaring of vertebral bodies
- Syndesmophytes → “bamboo spine”

Management
Pharmacological
- NSAIDs – First-line for pain and stiffness
- DMARDs (for peripheral joint involvement):
- Sulfasalazine, Methotrexate
- Biologics:
- Infliximab (TNF-α inhibitor)
Non-Pharmacological
- Physiotherapy & exercise: Maintain posture and mobility
- Postural training
- Surgical:
- Hip replacement
- Vertebral osteotomy (for severe kyphosis)
Complications
- Spinal deformity → kyphosis, disability
- Osteoporosis and increased fracture risk
- Reduced lung volumes due to chest wall rigidity
- Vision loss (if uveitis untreated)
- Aortic insufficiency
- Neurological compromise (due to spinal instability or fracture)
Differential Diagnosis
- Mechanical back pain
- Rheumatoid arthritis
- Psoriatic arthritis
- Reactive arthritis
- Diffuse idiopathic skeletal hyperostosis (DISH)
Summary – Ankylosing Spondylitis
Ankylosing spondylitis is a chronic inflammatory arthritis affecting the spine and sacroiliac joints, leading to progressive stiffness, fusion, and postural deformities. Associated with HLA-B27, it typically presents in young males with lower back pain and morning stiffness. Management involves NSAIDs, DMARDs, biologics, and physiotherapy. For further reading, visit our Musculoskeletal Overview page.