Table of Contents
Overview – Bony Injuries
Bony injuries encompass fractures, dislocations, and musculoskeletal emergencies that affect skeletal integrity and joint function. These injuries require prompt diagnosis and management to prevent infection, neurovascular compromise, permanent functional loss, or compartment syndrome. Medical students must recognise fracture patterns, describe radiological findings accurately, and understand treatment principles including reduction, immobilisation, and physiologic bone healing.
Definition
| Term | Definition |
|---|---|
| Fracture | A break in a bone |
| Compound Fracture | An open fracture where the skin is broken |
| Dislocation (Luxation) | Abnormal articulation due to joint surface displacement |
| Reduction | Restoring correct alignment of a fracture or dislocation |
| Splint | Device used to immobilise injured limb or spine |
| Neurovascular Compromise | Damage to surrounding vessels or nerves, risking loss of function |
| Compartment Syndrome | Bleeding/swelling within a muscle compartment causing compression |
Musculoskeletal Emergencies
Why Fractures Are Emergencies
- Open fractures risk infection
- Some fractures need reduction or surgery to heal
- Neurovascular compromise may cause irreversible damage
Why Dislocations Are Emergencies
- Delay in reduction increases difficulty and risks joint damage
- Risk of ligament rupture, impaired function
- Potential vessel and nerve compression
Dismemberment
- Major tissue loss or limb amputation → Permanent functional loss
Urgency Factors
- ABC compromise
- Active bleeding
- Vascular or nerve injury
- Open vs closed fracture
- Severe pain
- Risk of permanent loss of function
Musculoskeletal Emergency Priorities
- Primary Survey – ABCs first (“life before limb”)
- Identify the Injury
- Analgesia
- Splinting
- Prevent Infection
- Reduction if needed
Benefits of Reduction & Splinting
Splinting
- Reduces pain & bleeding
- Promotes healing
- Prevents further bone, neurovascular, and functional damage
Reduction
- Restores function & anatomy
- Reduces pain
- Prevents long-term compromise
Fracture Aetiology & Healing
Aetiology
- Trauma
- Pathological fractures: e.g., osteoporosis, bone metastases
Phases of Fracture Healing
| Phase | Timeframe | Process |
|---|---|---|
| 1. Haematoma & Inflammation | 1–3 days | Blood clot + fibrin mesh |
| 2. Soft Callus | 1–3 weeks | Granulation tissue + fibroblasts + osteoid deposition |
| 3. Hard Callus | 1–2 months | Mineralised osteoid (visible on X-ray) |
| 4. Remodelling | >2 months | Woven bone → lamellar bone |

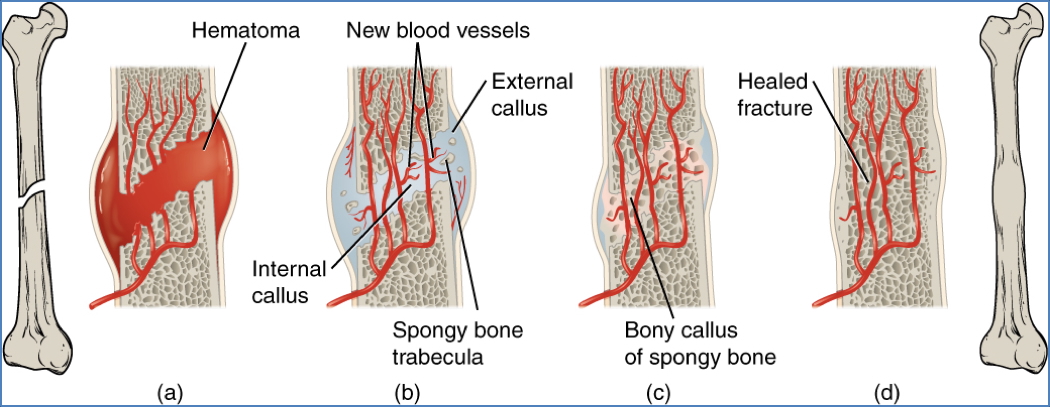
Bone Remodelling
- Driven by:
| Process | Cell Type | Function |
|---|---|---|
| Resorption | Osteoclasts | Destroy old bone |
| Apposition | Osteoblasts | Deposit new bone |

Clinical Features of Fractures
- Pain, swelling, loss of function
- Open fracture: risk of infection
- NV compromise → Nerve or artery compression/rupture
- Compartment syndrome → Risk of crush syndrome
Crush Syndrome: Muscle necrosis from compartment syndrome → DIC, rhabdomyolysis, amputation
Fracture Treatment
- Reduction (open or closed)
- Immobilisation (cast, splint, rod, pins)
- Analgesia
- Rest & rehabilitation (e.g., physiotherapy)
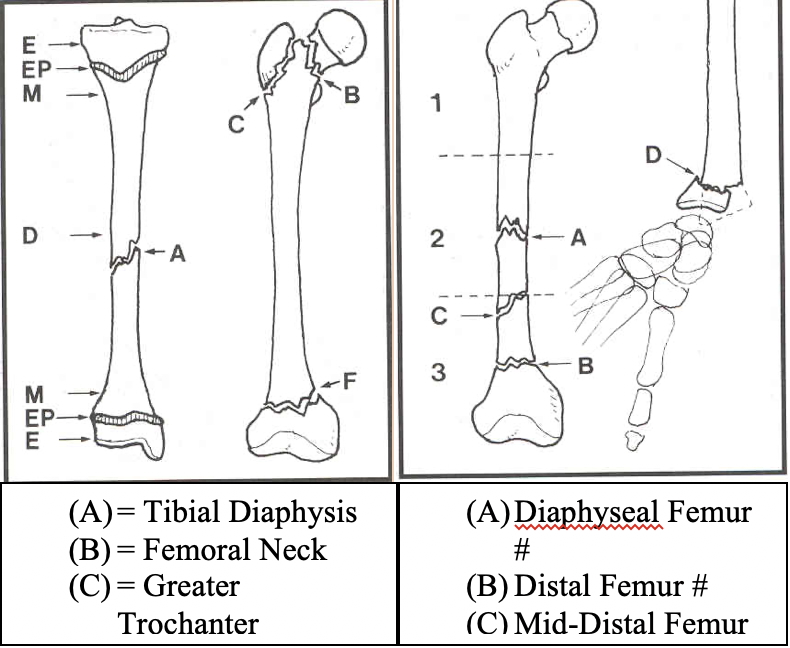
Describing a Fracture on X-Ray
- Fracture or Dislocation?
- Which Bone?
- Location of Injury?
| Term | Description |
|---|---|
| Epiphysis | Bone end |
| Epiphyseal Plate | Growth plate (children) |
| Metaphysis | Between diaphysis and epiphysis |
| Diaphysis | Shaft (split into proximal, mid, distal 1/3) |
| Epicondyle | Proximal joint landmarks |
| Malleolus | Ankle prominences |
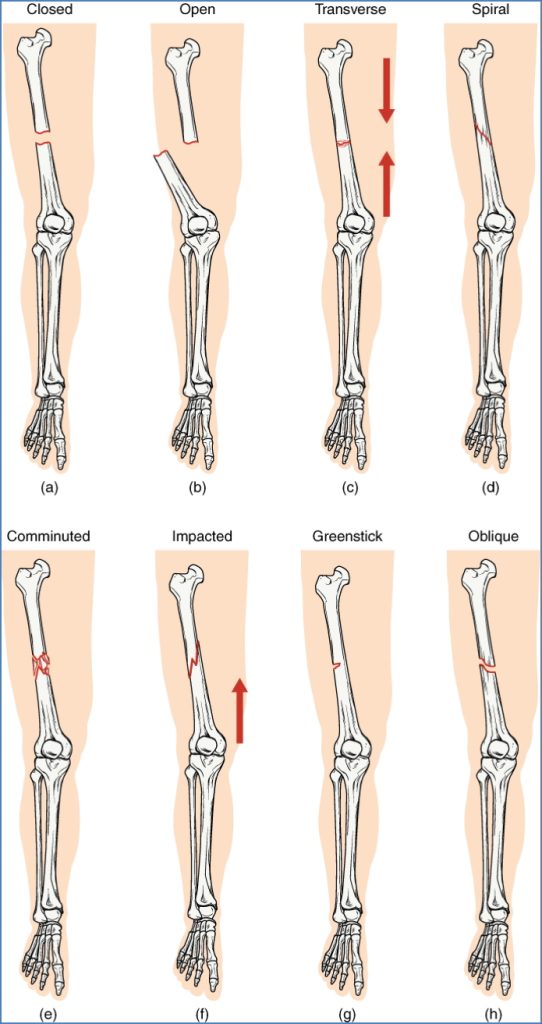
- Type of Fracture?
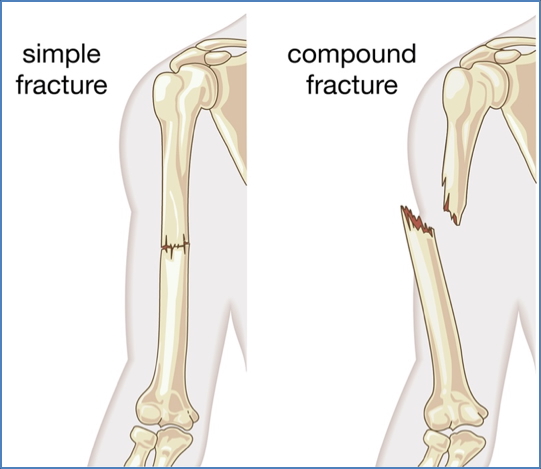
| Type | Description |
|---|---|
| Complete | Full separation of bone fragments |
| Incomplete | Partial separation (e.g. greenstick in children) |
| Transverse | Perpendicular to bone axis |
| Linear | Parallel to bone axis |
| Oblique | Angled across bone axis |
| Spiral | Curved pattern (often from twisting) |
| Greenstick | Partial break in flexible bone (common in children) |
| Comminuted | ≥3 bone fragments |
| Compacted | Fragments crushed into each other (common in hip) |

2. https://www.orthopedic-institute.org/fracture-care/types-of-fractures/
- Displacement?
- Described as % of offset between fragments (e.g. 50%, 100%)

- Angulation?
- Measured in degrees, e.g. “30° lateral angulation of distal femur”

- Rotation?
- Difficult to assess on plain film; inferred from clinical alignment

- Dislocation (Luxation)?
| Joint | Common Features |
|---|---|
| Shoulder | Most common; anterior dislocation often seen |
| Elbow/Wrist | Often with associated fractures |
| Fingers | IP joint involvement |
| Knee/Ankle | Often high-force injuries with fractures |
Direction of dislocation: anterior/posterior, superior/inferior

Summary – Bony Injuries
Bony injuries such as fractures and dislocations are common emergency presentations that can threaten function, vascular integrity, and even life. Proper assessment, early reduction, splinting, and awareness of complications like compartment syndrome are vital. Understanding the types, healing stages, and radiological descriptions is essential for medical students. For a broader context, see our Musculoskeletal Overview page.