Table of Contents
Overview – Rheumatoid Arthritis
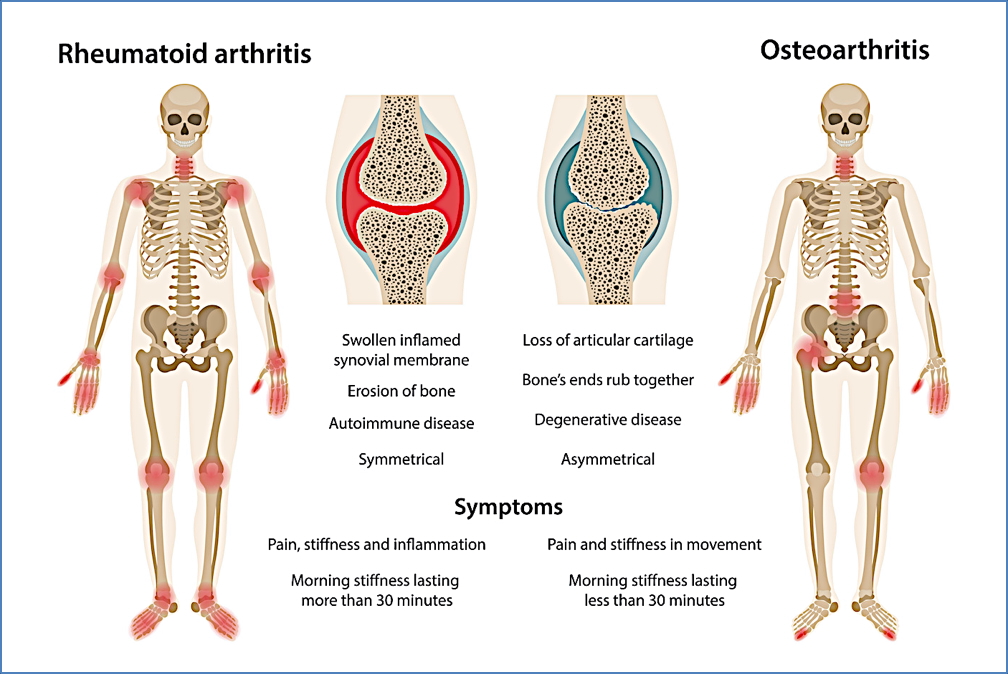
Rheumatoid arthritis (RA) is a chronic, systemic autoimmune disease that primarily targets synovial joints, causing symmetrical, polyarticular inflammation and joint destruction. RA is the most common form of inflammatory arthritis and affects young to middle-aged adults, especially women. The disease is characterised by morning stiffness, progressive joint deformity, and multi-organ involvement. Early diagnosis and treatment are essential to prevent long-term disability.
Definition
Rheumatoid arthritis is a seropositive, autoimmune, inflammatory arthritis that leads to chronic synovitis, joint destruction, and systemic manifestations. It typically involves the small joints of the hands in a symmetrical pattern.
Aetiology
- Genetic Autoimmune Disorder
- HLA-DR4 and HLA-DR1 associated
- Environmental triggers (e.g. smoking, infections)
- Autoantibody formation, notably:
- Rheumatoid factor (RF): IgM antibodies targeting Fc portion of IgG
- ACPA: Often detectable years before clinical onset
- Mechanisms include:
- Immune complex formation (RF:IgG) → deposition in joints
- Complement activation → chondrocyte lysis
- CD4 T-cell activation → macrophage cytokine release (TNFα, IL-1, IL-6)
- Osteoclast activation → bone erosion
- Plasma cell activation → sustained antibody production
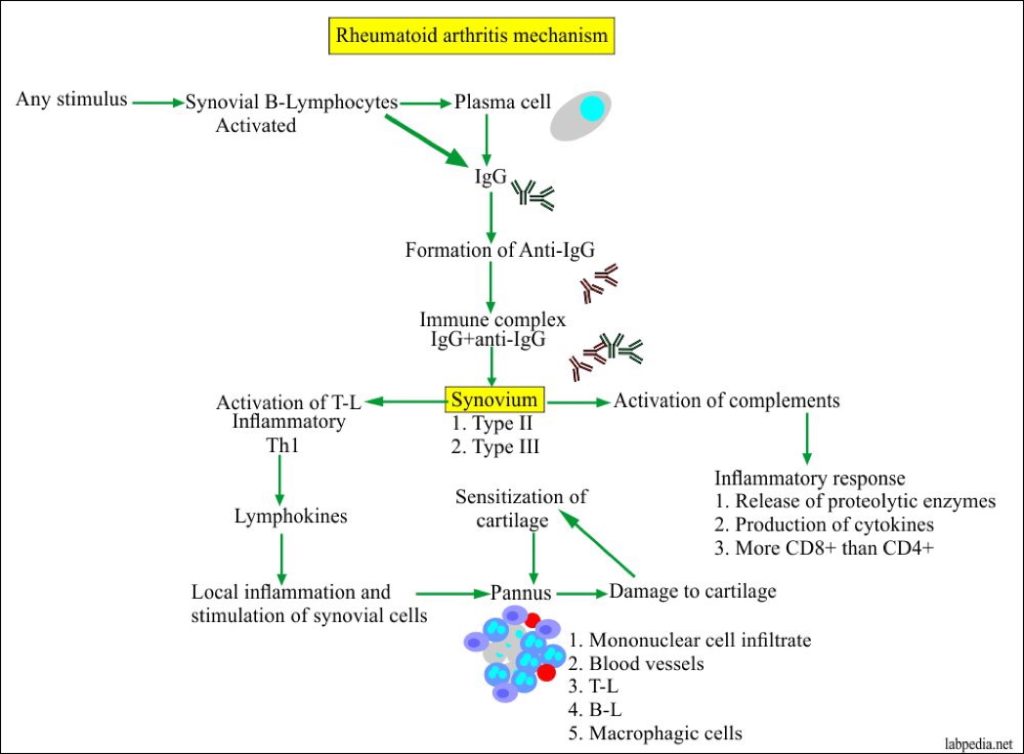
Pathogenesis
- Autoimmune activation → Rheumatoid Factor (IgM against IgG)
- Anti-CCP antibodies target citrullinated peptides
- Macrophage-mediated synovial inflammation → pannus formation
- Cartilage erosion, joint destruction, and fibrous ankylosis
Morphology
- Pannus: thickened, inflamed synovium with papillary projections
- Articular cartilage erosion
- Fibrous and bony ankylosis
- Joint deformity and subluxation


Clinical Features
- Age of onset: 20–40 years
- Pattern: Symmetrical polyarthritis, particularly MCP, PIP, and wrists
- Morning stiffness lasting >1 hour
- Joint findings:
- Joint pain, swelling, and morning stiffness
- Symmetrical involvement of small joints (hands and feet)
- Ulnar deviation, joint deformities
- Erosions visible on X-ray
- Functional disability and intrinsic muscle wasting
- Systemic involvement:
- Dermatologic: Rheumatoid nodules (commonly elbows)
- Vasculitis: Digital infarcts, gangrene
- Ophthalmologic: Dry eyes, scleritis
- Pulmonary: Fibrosis, pleural effusion, nodules
- Cardiac: Pericarditis, valvular disease
- GI: PUD (from NSAIDs), dry mouth
- Renal: Amyloidosis → proteinuria
- Liver: Portal fibrosis, nodular hyperplasia
- Neuro: Cervical spine instability, nerve entrapment
- Haematologic: Splenomegaly, lymphadenopathy, anaemia, leukopenia

Diagnosis
Diagnostic Criteria (≥4 required):
- Morning stiffness
- Arthritis of ≥3 joint areas
- Involvement of MCP, PIP or wrist joints
- Symmetrical arthritis
- Rheumatoid nodules
- RA seropositivity (RF)
- Radiographic erosions
Laboratory Tests
- Anti-Citrullinated Protein Antibody (ACPA/Anti-CCP)
- Highly specific
- May be positive years before onset
- Rheumatoid Factor (RF) – positive in ~70%
- ESR & CRP – non-specific inflammation markers
Differential Diagnosis
- Systemic lupus erythematosus (SLE)
- Psoriatic arthritis
- Reactive arthritis
- Osteoarthritis
- Gout
- Viral arthritis (e.g. parvovirus B19)
Management
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- COX inhibition → ↓ prostaglandin synthesis → pain/inflammation relief
Disease-Modifying Anti-Rheumatic Drugs (DMARDs)
- Methotrexate – inhibits folate metabolism, ↓ lymphocyte proliferation
- Sulfasalazine – anti-inflammatory and immunomodulatory
- Hydroxychloroquine – ↓ lysosomal acidity
- Leflunomide – inhibits pyrimidine synthesis
- Cyclosporin – blocks IL-2 receptor signalling
Corticosteroids
- Potent immunosuppressants
- Inhibit cytokine secretion and immune cell activation
- Used for acute flare control
Biologics
- Cytokine inhibitors:
- TNFα inhibitors
- IL-1 inhibitors
- IL-6 inhibitors
- Co-stimulation blockers (e.g. abatacept)
- Monoclonal antibodies targeting:
- B-cells (e.g. rituximab)
- Osteoclasts (prevent bone erosion)
- Pro-inflammatory cytokines
Complications
- Joint deformity and disability
- Atlantoaxial subluxation → spinal cord compression
- Extra-articular organ damage (lungs, heart, eyes)
- Amyloidosis
- Increased cardiovascular risk
Summary – Rheumatoid Arthritis
Rheumatoid arthritis is a seropositive autoimmune condition that causes chronic, symmetrical joint inflammation and systemic complications. Early recognition, serological testing, and initiation of DMARDs are critical to slowing progression and preserving joint function. For a broader context, see our Musculoskeletal Overview and Immune & Rheumatology Overview pages.