Table of Contents
Overview – Autonomic Nervous System Physiology
The physiology of the autonomic nervous system (ANS) governs involuntary functions of smooth muscle, cardiac muscle, and glands. It operates via reflex arcs and modulates organ function through a dual sympathetic-parasympathetic system. This article covers ANS neurotransmitters, receptors, drug targets, regulatory control, and clinical implications including tone, imbalance, and disease.
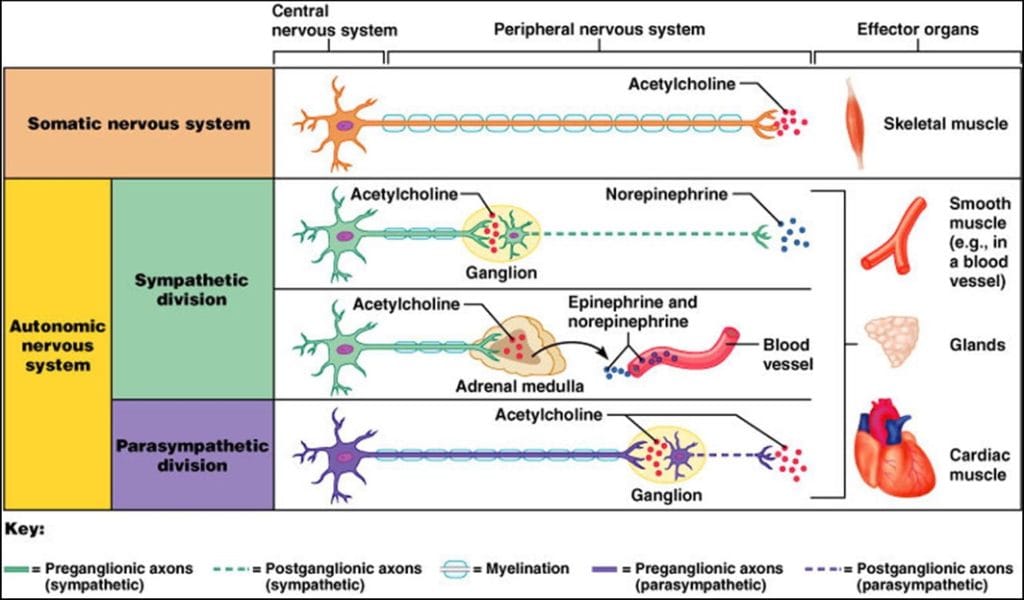
Neurotransmitters of the ANS
Afferent (Sensory) – PNS
- Glutamate, Calcitonin Gene-Related Peptide, Substance P
Efferent (Motor)
Somatic Division
- Neurotransmitter: Acetylcholine (ACh)
- Fibre: Thick, heavily myelinated → Fast conduction
- Effect: Always stimulatory
Autonomic Division
Preganglionic: Always ACh
Postganglionic:
- Sympathetic → Norepinephrine (NE)
- Parasympathetic → Acetylcholine (ACh)
- Adrenal Medulla: Releases NE + Epinephrine into bloodstream (stimulated by ACh)
Note: ANS fibres are thinner, less myelinated → slower conduction than somatic motor fibres
Receptors of the ANS
Cholinergic Receptors (ACh-sensitive)
1. Nicotinic Receptors
- Locations:
- Motor end plates of skeletal muscle
- Ganglionic neurons (both divisions)
- Adrenal medulla cells
- Mechanism: Ionotropic → ACh binding opens ion channels → always excitatory
2. Muscarinic Receptors
- Locations:
- Parasympathetic target organs
- Some sympathetic targets (e.g. sweat glands)
- Mechanism: Metabotropic → G-protein coupled → intracellular cascade
- Effect: Stimulatory or inhibitory depending on subtype:
- M1: Brain
- M2: Heart
- M3: Smooth muscle & glands
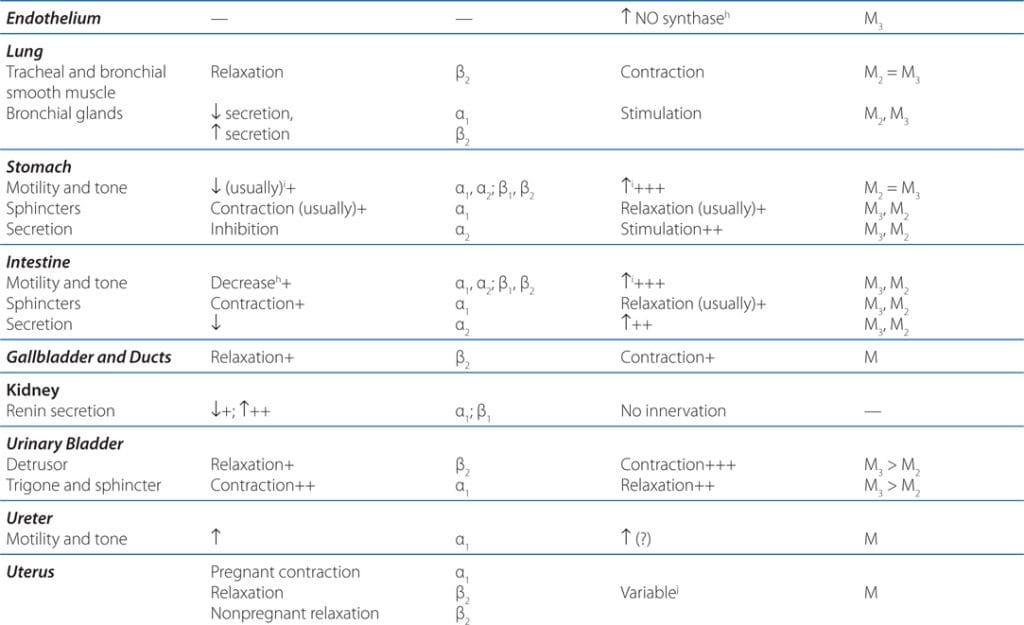
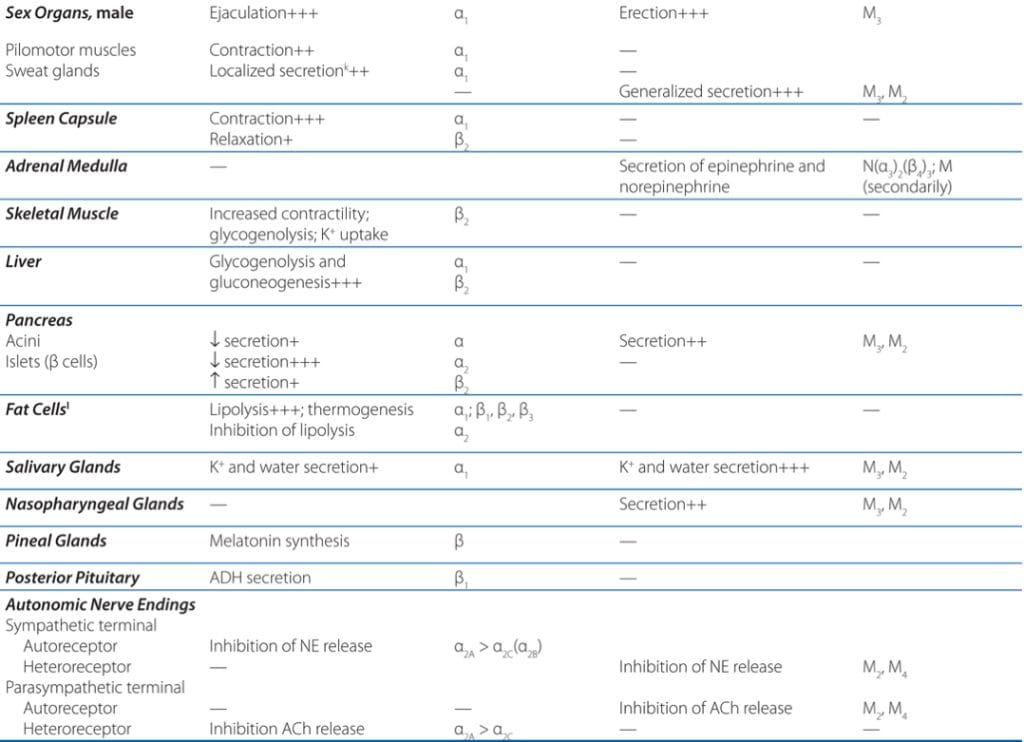
Adrenergic Receptors (NE/Epi-sensitive)
- Respond to norepinephrine and epinephrine
- Subtypes:
- Alpha: α1 / α2
- Beta: β1 / β2 / β3
- Effect: Depends on receptor type and organ distribution
- e.g. β1 = ↑HR; β2 = bronchodilation; α1 = vasoconstriction

Sympathetic & Parasympathetic Tone
Sympathetic (Vasomotor) Tone
- Maintains baseline vascular tone
- ↑Sympathetic firing → Vasoconstriction → ↑BP
- Alpha-blockers reduce this tone → useful for hypertension
Parasympathetic Tone
- Dominates at rest → ↓HR, promotes GI & urinary function
- Sympathetic input can override during stress
- Blocking parasympathetic tone → ↑HR, ↓GI motility, dry mouth
Unique Sympathetic Roles
- Organs with sympathetic-only innervation:
- Adrenal medulla
- Sweat glands
- Arrector pili (skin)
- Kidneys
- Most blood vessels
Additional Functions
- Thermoregulation: Vasodilation/sweating vs. vasoconstriction
- Renin release: ↑BP via RAAS
- Metabolism:
- ↑Cell metabolic rate
- ↑Blood glucose
- Mobilises lipids
- “Red alert” for skeletal muscle
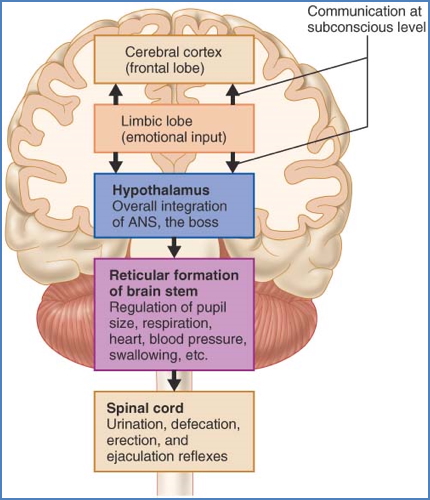
Central Control of the ANS
- Hypothalamus: Main integration centre
- Brainstem: Reflex centres for HR, BP, respiration, pupil size
- Spinal Cord: Autonomic reflexes (e.g. micturition)
Note: Limbic system modulates hypothalamic control during emotion (e.g. fear, anxiety)
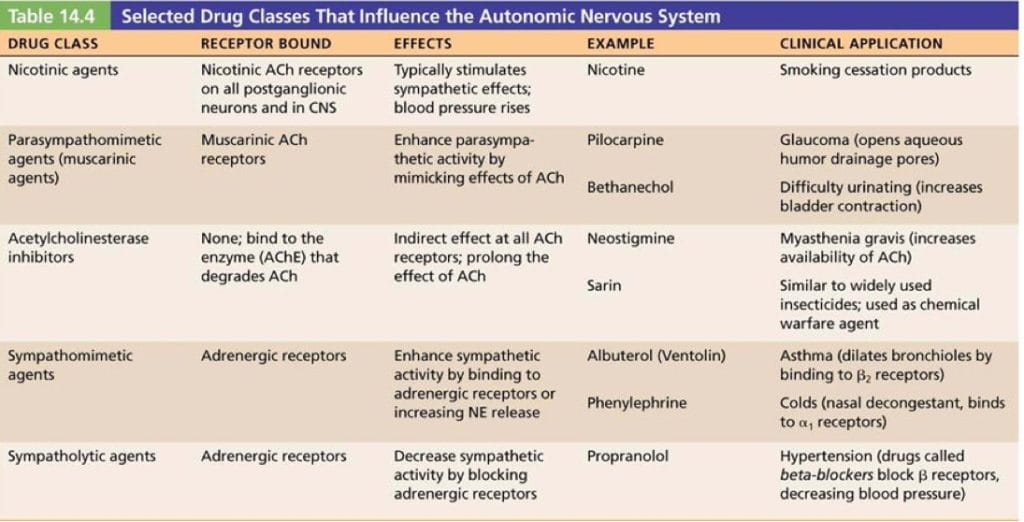
Clinical Applications & Drug Targets
Somatic Nervous System
- AChE Inhibitors → ↑ACh at neuromuscular junction
- Nicotinic Antagonists → e.g. Neuromuscular blockers (anaesthesia)
Autonomic Nervous System
Sympathetic
- Drugs that affect NE/Epi release or reuptake
- Adrenergic agonists/antagonists
- e.g. β-blockers for hypertension
Parasympathetic
- AChE inhibitors → e.g. Neostigmine
- Muscarinic agonists/antagonists
Ganglionic Blockers
- Block all autonomic output
- Effect depends on dominant tone in each tissue
- e.g. vasodilation in sympathetically-dominant blood vessels

ANS Disorders & Homeostatic Imbalances
Disorders
- Inflammatory: Guillain-Barre, Myasthenia Gravis
- Metabolic: Diabetic neuropathy, vitamin deficiencies
- Toxic: Alcohol, urea
- Infectious: Shingles, diphtheria
- Genetic/Traumatic: Nerve injuries, hereditary neuropathies
Imbalances
- Hypertension: Chronic sympathetic activation
- Treat with β-blockers, adrenergic antagonists
- Raynaud’s disease: Exaggerated vasoconstriction response
- Autonomic dysreflexia: Life-threatening sympathetic surge in quadriplegia
Summary – Autonomic Nervous System Physiology
Autonomic physiology involves a complex interaction of neurotransmitters (ACh, NE, Epi), receptor types (nicotinic, muscarinic, adrenergic), and central modulation. Its balance maintains visceral function, while disruptions contribute to major clinical conditions. For a broader context, see our Nervous System Overview page.