Table of Contents
Overview – Dementias
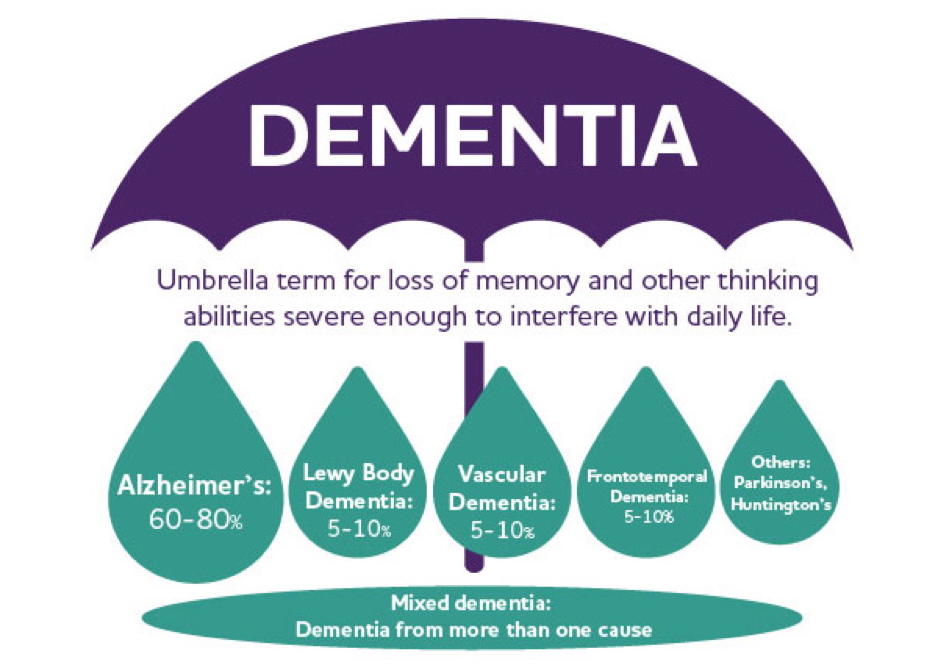
Dementias are a group of acquired, progressive neurodegenerative conditions characterised by global cognitive decline without altered consciousness. Common forms include Alzheimer’s disease, Lewy body dementia, frontotemporal dementia (Pick’s disease), vascular dementia, and age-related senile dementia. Each has unique pathophysiological mechanisms and clinical features. Understanding the distinctions between these syndromes is crucial for diagnosis and management in clinical practice.
Definition
- Dementia = Acquired global impairment of intellect without altered level of consciousness
- Symptoms affect memory, cognition, executive function, language, behaviour
Epidemiology
- Affects ~5% of people >55 years
- 20% prevalence by age 80
- Risk doubles every 5 years past age 60
- 50% have associated behavioural/psychological symptoms
Clinical Diagnosis
- Gradual cognitive decline (starting with memory)
- Behavioural/psychiatric features (agitation, hallucinations, etc.)
- Progressive impact on ADLs (medications, finances, mobility)
- Cognitive screening: MMSE, MOCA
Alzheimer’s Disease
Aetiology
- Most common dementia type
- Multifactorial: genetic and environmental risk
- Early onset in Down syndrome
Pathophysiology
- ↑ β-amyloid → extracellular plaque deposition
- → Neuronal death and synaptic loss
- Also causes cerebral amyloid angiopathy

Mikael Häggström and brainmaps.org, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons
Morphology
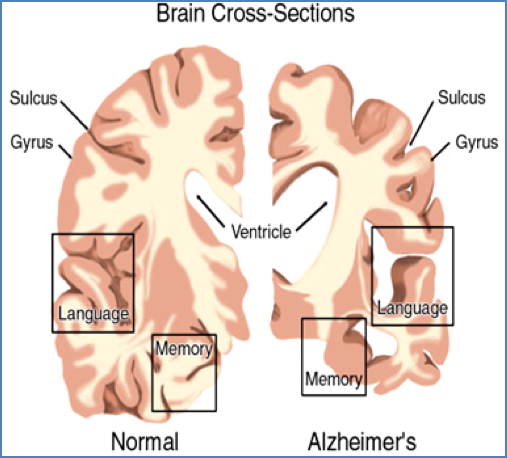
- Severe cortical atrophy, widened sulci, narrow gyri
- Compensatory ventricular dilation (hydrocephalus ex-vacuo)
Clinical Features
- Insidious onset (progresses over years)
- Early: short-term memory loss (hippocampal atrophy)
- Moderate: confusion, language difficulty, apathy
- Late: incontinence, seizures, global dysfunction
Management
- Acetylcholinesterase inhibitors (e.g. donepezil)
- Supportive care
Prognosis
- Mean survival ~7 years from diagnosis
- Common cause of death: aspiration pneumonia

Lewy Body Dementia
Aetiology
- Unknown; may have genetic predisposition
Pathophysiology
- α-synuclein aggregates (Lewy bodies) throughout cortex
- Neuronal degeneration in limbic and cortical areas
Morphology
- Cortical atrophy, especially in frontal/temporal regions
Clinical Features
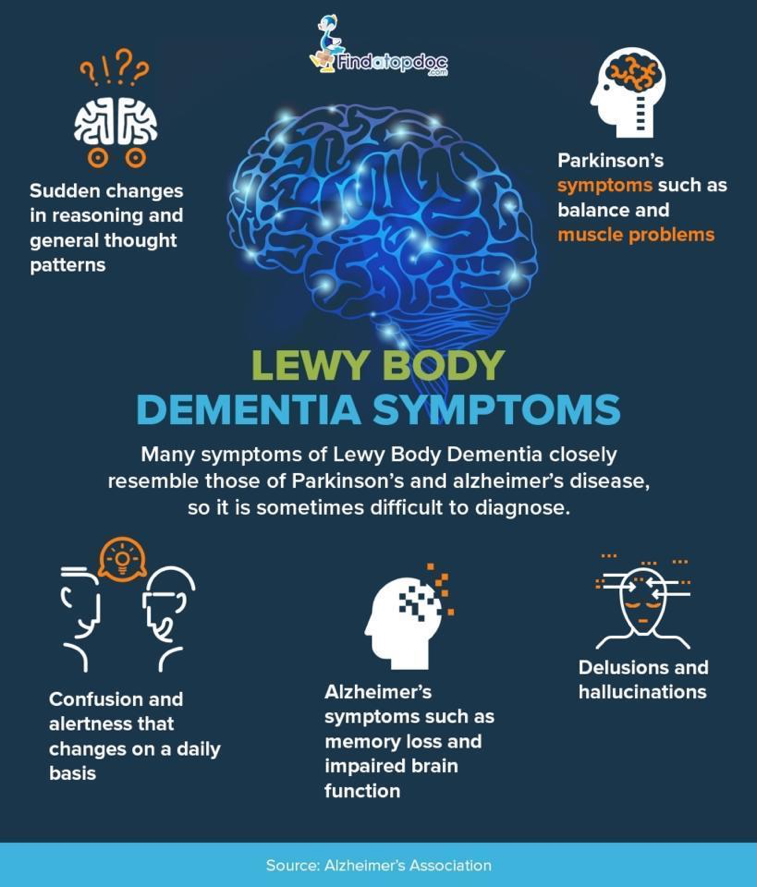
- Rapid progression (months)
- Fluctuating cognition
- Early visual hallucinations (faces, animals, children)
- Parkinsonism (shuffling gait, cogwheel rigidity)
- Delusions, transient altered consciousness
Management
- Cholinesterase inhibitors (some benefit)
- Avoid antipsychotics (may worsen symptoms)
Frontotemporal Dementia (incl. Pick’s Disease)
Aetiology
- “Pick’s disease”: unknown
- Other FTDs often genetic
Pathophysiology
- Intracellular tau protein accumulation → selective frontal and temporal lobe atrophy
Morphology
- Marked frontal and temporal lobe atrophy
- Parietal and occipital lobes spared

Clinical Features
- Onset between 40–65 years
- Behavioural change precedes memory loss (key distinguishing feature)
- Disinhibition, poor impulse control
- Progressive aphasia (expressive and receptive)
- Preserved memory until late

Vascular Dementia (Multi-Infarct Dementia)
Aetiology
- 2nd most common form
- Due to cumulative brain ischaemia from:
- Hypertension
- Atherosclerosis
- Strokes/TIAs
Pathophysiology
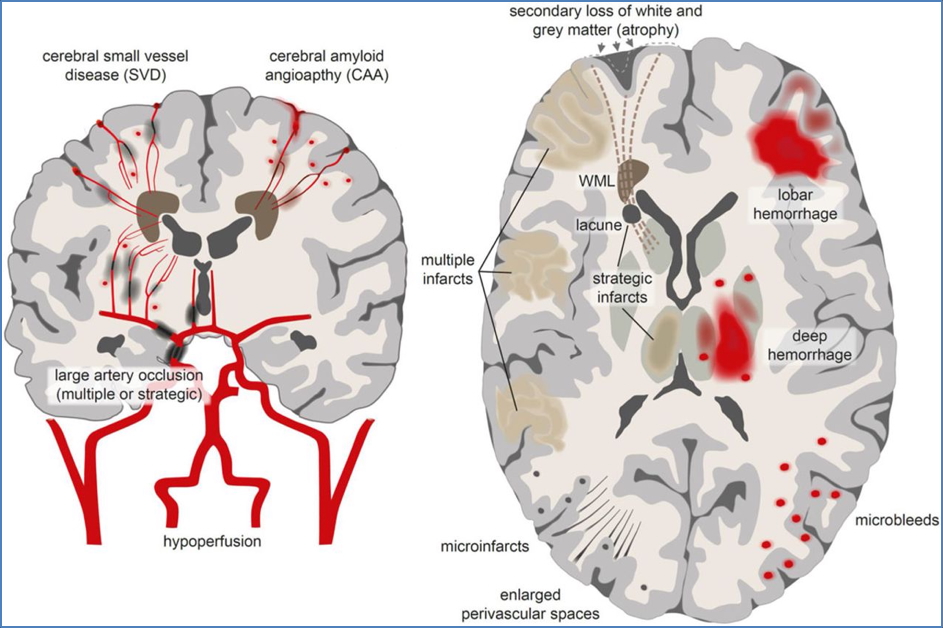
- Stepwise decline after successive CVAs
- May be single large infarct or multiple small infarcts
- Lacunar infarcts, cortical necrosis common
Morphology
- Infarcts visible on MRI/CT
- Lacunar changes, white matter disease
Clinical Features
- Memory loss, poor attention
- Executive dysfunction → impaired ADLs
- History of stroke or vascular risk factors
- Parkinsonism (shuffling gait)
Management
- Preventative only:
- BP control, lipid management
- Antiplatelet therapy
- Lifestyle modification
Age-Related (Senile) Dementia
Aetiology
- Neuronal atrophy due to ageing
Pathophysiology
- Generalised loss of cortical neurons
- ↓ Dendritic branching
- ↑ Gliosis (neurons replaced by glial cells)
Morphology
- Cortical thinning
- Ventricular enlargement
- Thickening of leptomeninges
Clinical Features
- Global cognitive impairment
- Slow progression
- No clear histopathological lesion
Wernicke-Korsakoff Syndrome
Aetiology
- Chronic alcohol use → thiamine (vitamin B1) deficiency
Pathophysiology
- ↓ Thiamine → ↓ glucose metabolism → ATP depletion → neuronal damage
- Mammillary body, cerebellum, cortex affected
Morphology
- Mammillary body atrophy and haemorrhage
- Cerebellar and cortical atrophy
Clinical Features
- Confusion, ataxia, nystagmus
- Anterograde + retrograde amnesia
- Confabulation
- Gait disturbance
Management
- IV thiamine before glucose
- Add vitamin B12 to prevent subacute combined degeneration

Dementia Pugilistica (Chronic Traumatic Encephalopathy)
Aetiology
- Repetitive head trauma (e.g. contact sports)
Pathophysiology
- Repeated sub-concussive injury → axonal damage, gliosis, neurodegeneration
Morphology
- Hydrocephalus
- Thinning of corpus callosum
- Cerebellar atrophy
Clinical Features
- Gait ataxia
- Cognitive decline
- Dysphasia
- Parkinsonism
- Personality changes

Summary – Dementias
Dementias are a spectrum of neurodegenerative disorders with distinct pathological and clinical profiles. Alzheimer’s disease is the most common, but vascular, Lewy body, and frontotemporal dementias are also important to recognise. Each form has unique diagnostic features and management strategies. For a broader context, see our Nervous System Overview page.