Table of Contents
Overview – Intracranial Haemorrhages
Intracranial haemorrhages are acute neurological emergencies caused by bleeding within the skull. They can result from trauma, vascular malformations, aneurysmal rupture, or chronic hypertension. The four major types—epidural, subdural, subarachnoid, and intracerebral—have distinct causes, anatomical locations, clinical courses, and imaging findings. Early recognition and targeted management are crucial to reduce morbidity and mortality.
Aetiology
| Cause | Haemorrhage Type |
|---|---|
| Skull fracture (trauma) | Epidural haemorrhage |
| Low-force trauma (esp. elderly) | Subdural haemorrhage |
| Congenital berry aneurysm | Subarachnoid haemorrhage |
| AV malformations | Intracerebral haemorrhage |
| Hypertension | Intracerebral haemorrhage (spontaneous) |
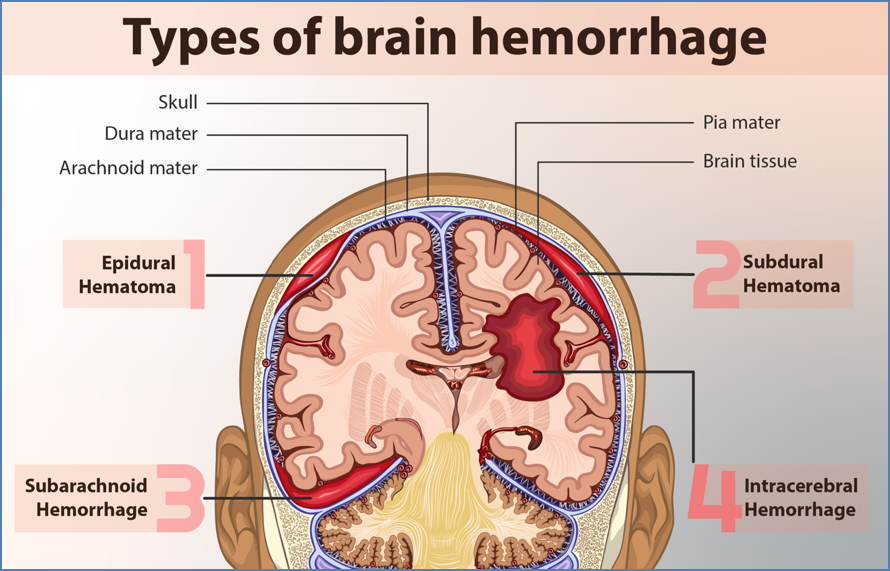
Epidural (Extradural) Haemorrhage
Aetiology & Pathogenesis
- Caused by arterial rupture (usually middle meningeal artery) due to skull fracture
- Blood accumulates between dura mater and skull, splitting the dura under high pressure
Morphology
- Biconvex (lens-shaped) haematoma on CT
- Bleeding limited by dural attachments
- Compression of underlying brain
Clinical Course
- Rapid onset:
- Initial LOC
- Lucid interval
- Sudden deterioration (herniation signs)
Signs & Symptoms
- Severe headache, vomiting, altered consciousness
- Ipsilateral fixed/dilated pupil (CN III compression)
- Contralateral hemiparesis
- Potential for uncal/tonsillar herniation → coma/death
Investigations
- CT Head: Hyperdense, biconvex shape (does not cross suture lines)
Management
- Urgent neurosurgery: Burr hole ± craniotomy
- Excellent prognosis if treated promptly
- Untreated → brain herniation and death

Subdural Haematoma
Aetiology & Pathogenesis
- Venous bleed from bridging veins, usually due to low-impact trauma
- Blood collects between dura mater and arachnoid mater
Morphology
- Crescent-shaped haematoma on CT
- Can spread across hemispheres
- Brain atrophy common (elderly, alcoholics)
Clinical Course
| Type | Presentation | Progression |
|---|---|---|
| Acute | Immediate symptoms after trauma | Rapid deterioration, high mortality |
| Chronic | Days–weeks later | Gradual onset headache, confusion, focal signs, seizures |
Signs & Symptoms
- Somnolence, dizziness, ataxia
- Confusion, amnesia, visual changes
- Weakness, nausea, seizures
- More subtle in chronic cases
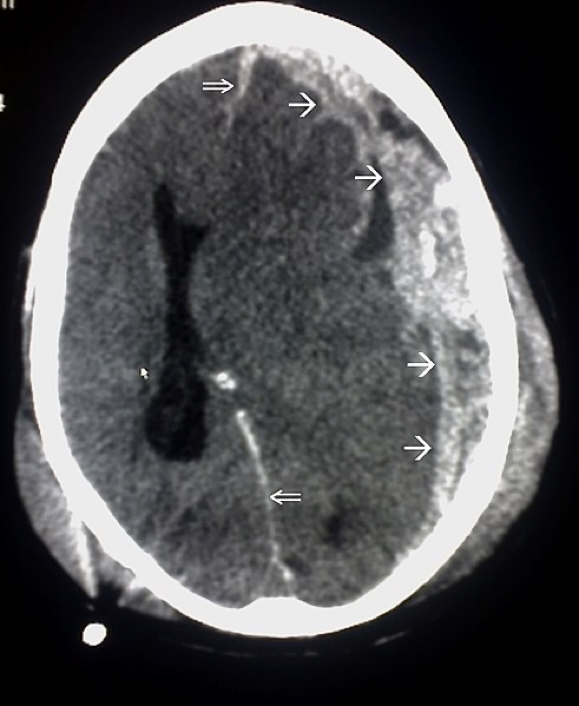
Investigations
- CT Head:
- Acute: Crescent-shaped density
- Chronic: Hypodense, follows brain contour
- Midline shift may be present
Management
- Severe cases: Burr hole drainage
- Small/chronic cases: Conservative ± serial imaging
- Prognosis often poorer due to underlying cerebral atrophy
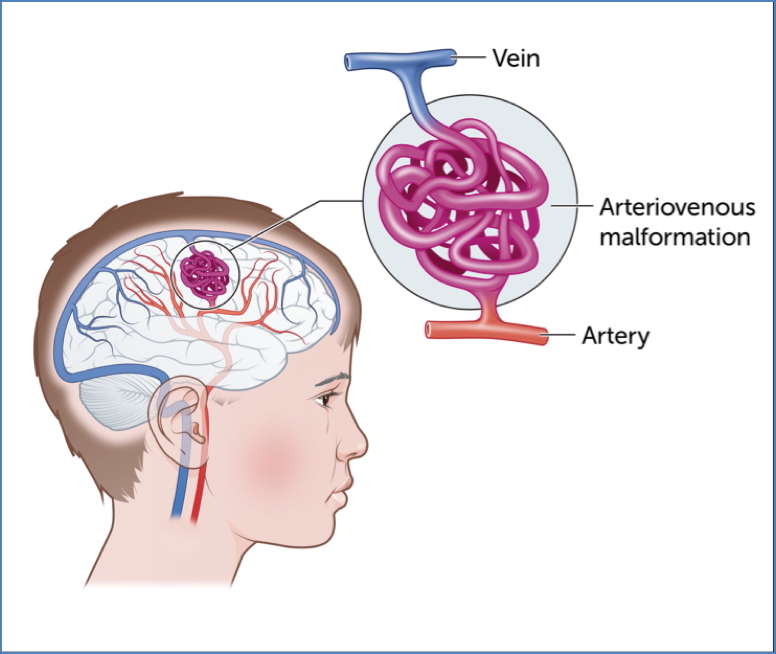
Subarachnoid Haemorrhage
Aetiology & Pathogenesis
- Rupture of berry aneurysm in Circle of Willis
- Common sites: MCA > ACA > PCA
- Blood enters the subarachnoid space, mixing with CSF
- May be precipitated by hypertension
Morphology
- Blood in sulci and basal cisterns
- Can appear in ventricles if severe

Clinical Features
| Phase | Symptoms |
|---|---|
| Pre-rupture | Headache, balance issues, dysphasia |
| Post-rupture | “Thunderclap headache”, vomiting, meningism, hemiparesis, diplopia, seizures, ALOC |
Investigations
- CT Head: Blood in sulci and fissures
- Lumbar puncture: Xanthochromia (if CT negative)
- CT Angiography: To identify aneurysm
Management
- Stabilise: Airway, breathing, circulation, ICU care
- Neurosurgical referral (clipping/coiling)
- Control ICP (mannitol, hyperventilation, corticosteroids)
Prognosis
- <50% survival
- High morbidity in survivors (vasospasm, hydrocephalus, seizures)


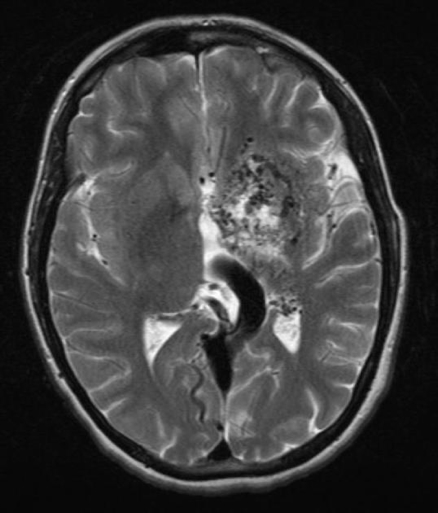
Intracerebral Haemorrhage
Aetiology
- Hypertension (most common)
- AV malformations, trauma, bleeding diathesis
Pathogenesis
- Bleeding into brain parenchyma
- Leads to mass effect, ↑ICP, and ischaemia
Morphology
- Slit haemorrhages in chronic HTN
- Lacunar infarcts in brainstem/basal ganglia
Clinical Features
- Acute headache, vomiting, meningism
- Nystagmus, anisocoria, focal neurological deficits
- Signs of raised ICP and possible brain herniation
- Altered consciousness
Investigations
- CT/MRI Brain: Confirms haemorrhage
- Transcranial Doppler: Assess AVMs
Management
- Supportive: Ventilation, BP control
- Mannitol, corticosteroids for ICP
- Surgery if >3cm or herniation
- Correct coagulopathy if present
Prognosis
- 40% mortality
- Most survivors have permanent disability
Summary – Intracranial Haemorrhages
Intracranial haemorrhages are classified by anatomical location into epidural, subdural, subarachnoid, and intracerebral types, each with unique causes, clinical features, and imaging appearances. Rapid diagnosis with CT, close monitoring for signs of raised ICP, and timely neurosurgical intervention are key to improving outcomes. For a broader context, see our Nervous System Overview page.