Table of Contents
Overview – Ischaemic Encephalopathy
Ischaemic encephalopathy, also known as hypoxic-ischaemic brain injury, results from a critical reduction in oxygen or perfusion to the brain. This global cerebral ischaemia most commonly arises in cardiac arrest, shock, or severe hypoxaemia, and its effects range from transient confusion to irreversible coma. Understanding the pathophysiology, especially the vulnerability of selective brain regions, is essential in clinical neurology and ICU contexts.
Definition
- Ischaemic Encephalopathy refers to diffuse brain injury caused by global cerebral hypoperfusion or hypoxia.
- Not a stroke (which is focal); this is a global event, often seen in systemic collapse.
Aetiology
| Mechanism | Examples |
|---|---|
| ↓ Cerebral Perfusion | Heart failure, hypotension, shock, carotid occlusion |
| ↓ Oxygen Carrying Capacity | Anaemia, respiratory failure, hypoxaemia |
| ↓ Oxygen Utilisation | Cyanide poisoning, carbon monoxide poisoning |
| ↑ Metabolic Demand | Generalised seizures, status epilepticus |
Pathophysiology
- Systemic compromise → ↓ blood flow or oxygen → global cerebral ischaemia
- Selective vulnerability of neurons in metabolically active brain regions
Vulnerable Areas
| Age Group | Sensitive Regions |
|---|---|
| Adults | – Watershed zones (ACA–MCA borders) – Cortical layers III, V, VI – Hippocampus – Cerebellar Purkinje Cells |
| Infants | – Brainstem nuclei |
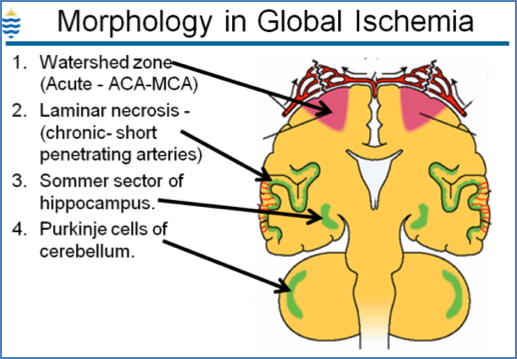
Morphology
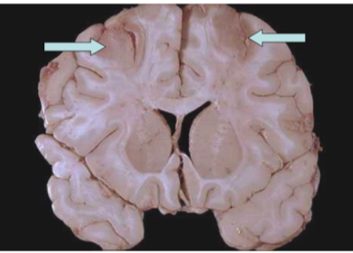
- Watershed infarcts: Wedge-shaped necrosis between ACA & MCA territories
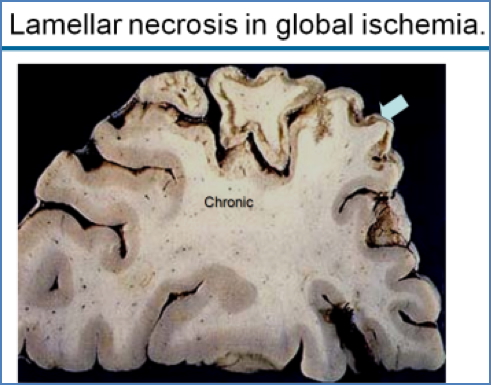
- Laminar necrosis: Cell death in specific cortical layers (especially III, V, VI)
- Hippocampal damage: Memory and learning deficits
- Purkinje cell necrosis: Cerebellar dysfunction
Clinical Features
| Severity | Presentation |
|---|---|
| Mild | Transient confusion, delayed reaction time |
| Moderate | Cognitive impairment, agitation, delayed recovery |
| Severe | Persistent vegetative state, coma, brain death (flat EEG) |
Summary – Ischaemic Encephalopathy
Ischaemic encephalopathy is a global brain injury caused by inadequate cerebral oxygen delivery. Cardiac arrest, anaemia, or poisoning may all contribute to this condition. The hippocampus, Purkinje cells, and watershed zones are especially sensitive to hypoxia. Clinical outcomes vary from reversible confusion to irreversible brain death. For a broader context, see our Nervous System Overview page.