Table of Contents
Overview – Multiple Sclerosis
Multiple sclerosis (MS) is a chronic, immune-mediated disease of the central nervous system that causes patchy demyelination in the brain and spinal cord. It typically presents in young adults and follows a relapsing-remitting or progressive course. Clinical features depend on the CNS regions affected but often include limb weakness, optic neuritis, and sensory changes. This article provides a concise overview of multiple sclerosis for final-year medical students, with a focus on pathology, diagnosis, and prognosis.
Definition
Multiple sclerosis is a chronic autoimmune demyelinating disorder of the central nervous system characterised by white matter lesions, which result in neurological deficits that relapse and remit or progressively worsen.
Aetiology
- Autoimmune inflammatory disorder of unknown trigger
- Genetic predisposition (e.g. HLA-DRB1 association)
- Environmental factors: Vitamin D deficiency, EBV infection, smoking
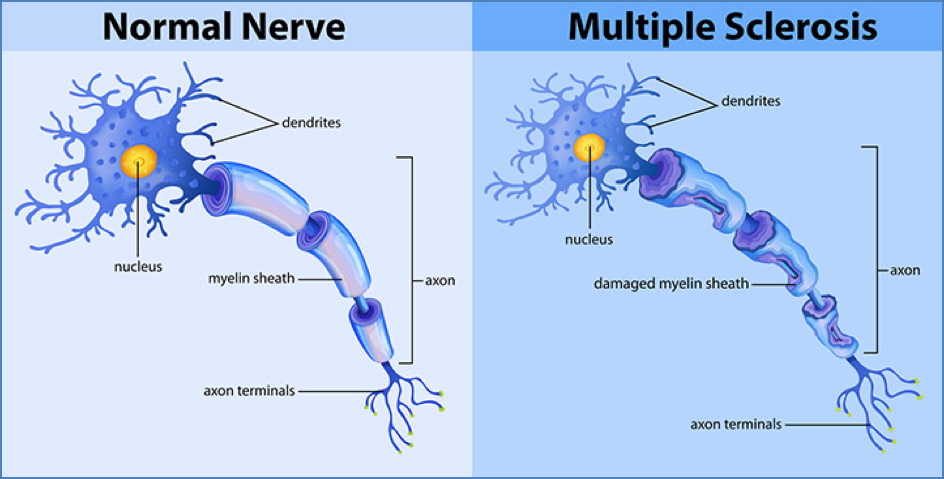
Pathophysiology
- T-cell mediated attack on oligodendrocytes and myelin
- Demyelination in the CNS → impaired nerve conduction
- Inflammation leads to:
- Axonal damage
- Gliosis (scar formation)
- Plaque formation, especially periventricular white matter
Morphology
Macroscopic
- Multiple plaques of demyelination, especially around ventricles
- Plaques appear as pink-grey lesions in white matter
Microscopic
- Perivascular infiltrates (T-cells, macrophages, plasma cells)
- Loss of myelin with relative axonal preservation
- Reactive gliosis surrounding demyelinated zones

Clinical Features
- Typical onset: Age 20–40 years
- Relapsing-remitting course (most common), or progressive
- White matter symptoms:
- Limb weakness
- Ataxia
- Paraesthesia
- Optic neuritis (e.g. blurred vision, eye pain)
- Internuclear ophthalmoplegia
- Vertigo and nystagmus (without tinnitus or deafness)
- Late-stage: Spastic quadriparesis → respiratory failure → pneumonia
Investigations
- MRI brain and spine: Multiple white matter plaques, especially periventricular
- CSF analysis:
- Oligoclonal IgG bands (indicative of intrathecal synthesis)
- Evoked potentials: delayed conduction time
Diagnosis
- Clinical + Radiological criteria
- Requires evidence of:
- Dissemination in space (multiple CNS locations)
- Dissemination in time (more than one episode)
Management
- Currently incurable
- Supportive care:
- Physiotherapy, occupational therapy, psychosocial support
- Acute relapses:
- High-dose corticosteroids
- Disease-modifying therapies:
- Immunomodulators (e.g. interferon-beta, glatiramer acetate, natalizumab)
- Aim to reduce relapse rate and delay progression
Complications
- Spasticity
- Urinary retention or incontinence
- Chronic fatigue
- Depression
- Pneumonia due to chest muscle paralysis (end-stage)
Differential Diagnosis
- Neuromyelitis optica
- Acute disseminated encephalomyelitis (ADEM)
- CNS vasculitis
- B12 deficiency
- HIV-related CNS disease
Summary – Multiple Sclerosis
Multiple sclerosis is a chronic autoimmune condition causing patchy CNS demyelination, most often in young adults. Its relapsing-remitting or progressive course leads to varied neurological symptoms, including limb weakness and optic neuropathy. Diagnosis is clinical, supported by MRI and CSF findings. For a broader context, see our Nervous System Overview page.