Table of Contents
Overview – Myasthenia Gravis
Myasthenia gravis is a chronic autoimmune disorder that causes fluctuating skeletal muscle weakness due to impaired neuromuscular transmission. It arises from autoantibodies that target the acetylcholine receptors at the neuromuscular junction. Classically, the weakness worsens with exertion and improves with rest. Understanding the pathophysiology, diagnostic strategies, and treatment options is essential for recognising and managing this potentially life-threatening condition.
Definition
Myasthenia gravis (MG) is an autoimmune disorder of the neuromuscular junction characterised by fatigable skeletal muscle weakness, most commonly involving the ocular and bulbar muscles.
Pathophysiology
- Autoantibodies attack acetylcholine receptors (AChRs) or related proteins (e.g. MuSK) at the neuromuscular junction → impaired synaptic transmission
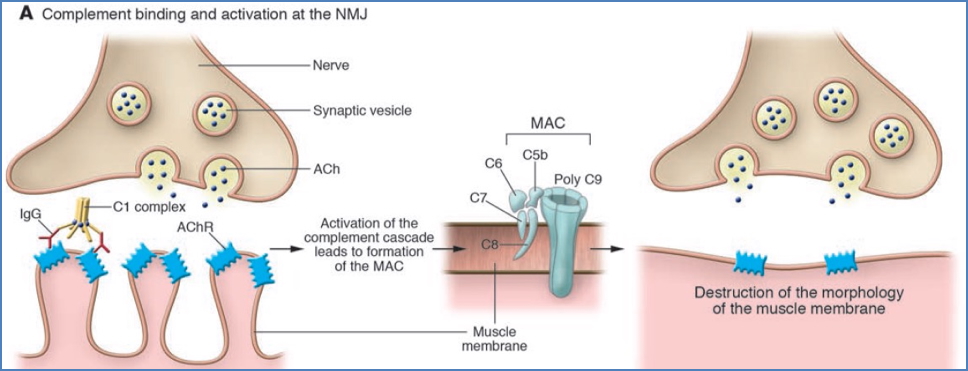
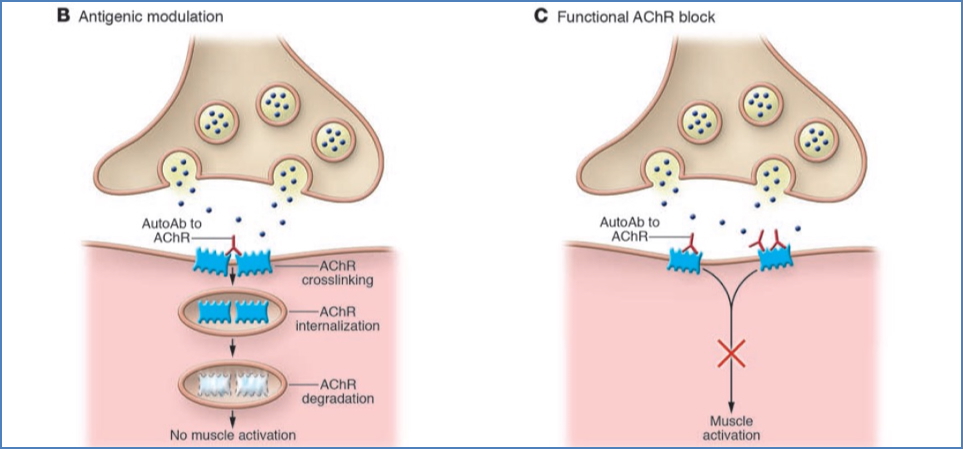
- Three mechanisms:
- 1. Complement-mediated destruction of AChRs → membrane damage
- 2. Antigenic modulation → cross-linking and internalisation of AChRs
- 3. Functional AChR blockade → prevents ACh from binding
- Result: ↓ AChR density → transmission failure → muscle weakness
Types of Myasthenia Gravis
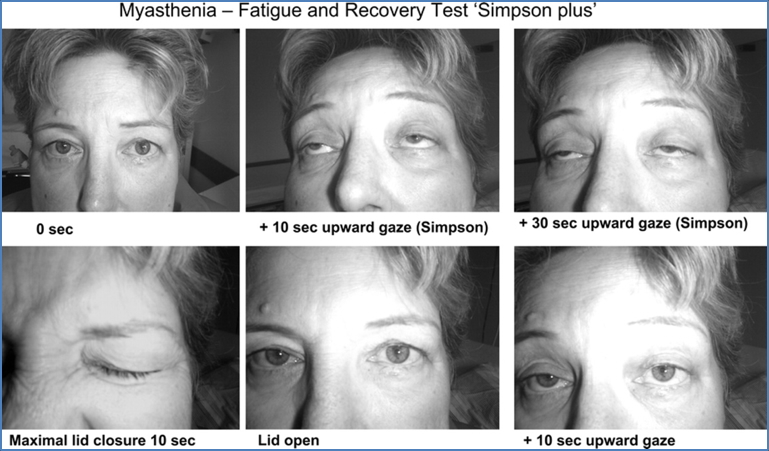
Ocular Myasthenia Gravis
- Affects only extraocular muscles
- Symptoms:
- Diplopia (double vision)
- Ptosis (drooping eyelid)
- Often a precursor to generalised MG
Generalised Myasthenia Gravis
- Widespread muscle weakness including:
- Limb girdles
- Bulbar muscles (swallowing, speaking)
- Facial muscles
- Respiratory muscles
- Symptoms:
- Waddling gait
- Limb weakness
- Dysphagia, dysarthria
- Dyspnoea
Diagnosis
- Edrophonium test (short-acting ACh-E inhibitor): transient symptom improvement
- Serology:
- Anti-AChR antibodies (most common)
- Anti-MuSK antibodies
- Electrophysiological testing:
- Repetitive nerve stimulation
- Single-fibre EMG (most sensitive)
Management
Symptomatic
- Acetylcholinesterase inhibitors (e.g. pyridostigmine):
- ↑ ACh levels in synapse → prolonged stimulation of AChRs
- Side effects (due to excess parasympathetic activity):
- Diarrhoea, bradycardia, bronchoconstriction, miosis
- Risk of cholinergic crisis with overdose
Immunomodulatory
- Thymectomy
- Plasma exchange or IVIG (especially in crisis)
- Immunosuppressants:
- Prednisone
- Azathioprine (purine analogue → ↓ B/T cell proliferation)
Crises
Cholinergic Crisis
- Caused by overdose of ACh-E inhibitors
- Excessive ACh → receptor desensitisation
- Presents with:
- Muscle weakness
- Bronchorrhoea, bradycardia, miosis
- Management: Stop ACh-E inhibitors
Myasthenic Crisis
- Due to progression of disease
- Severe muscle weakness, often involving respiratory muscles
- Management: Increase ACh-E inhibitor dose ± IVIG/plasmapheresis
Complications
- Respiratory failure (in crisis)
- Dysphagia → aspiration risk
- Long-term steroid use side effects
- Psychosocial impact (fatigue, appearance, QoL)
Differential Diagnosis
- Lambert-Eaton syndrome
- Botulism
- Mitochondrial myopathy
- Stroke
- Thyroid eye disease (in ptosis)
Summary – Myasthenia Gravis
Myasthenia gravis is a chronic autoimmune disorder causing fatigable weakness due to antibody-mediated disruption of neuromuscular transmission. It presents with ocular or generalised muscle weakness and may escalate to respiratory compromise. Management includes cholinesterase inhibitors, immunotherapy, and thymectomy. For a broader context, see our Nervous System Overview page.