Neurological patterns refer to recognizable symptom combinations that point towards specific underlying neurological conditions. Understanding common neuro-patterns is critical for diagnosis, especially in acute settings, such as headaches with red flag features, gait abnormalities, visual field defects, or signs of upper versus lower motor neuron lesions. This guide to neurological patterns helps final-year medical students efficiently differentiate causes by anatomical lesion location and functional impact.
Pattern Key Features Likely Diagnosis Isolated Severe Headache Acute onset, thunderclap pain, vomiting, meningism, ALOC Subarachnoid Haemorrhage Headache post-head injury (acute) LOC → lucid interval → deterioration, vomiting, seizures Extradural Haemorrhage Headache post-head injury (delayed) Worsening headache over days-weeks Subdural Haematoma Subacute Headache Headache + fever, photophobia, rash, nausea/vomiting Meningitis, Encephalitis Chronic/Recurrent Muscle tension, migraine, sinus pressure Tension Headache, Migraine, Sinusitis Pressure Headache Worse lying down, coughing, sneezing, vomiting ↑ICP from SOL Scalp Tenderness (elderly) Scalp vessel tenderness, new headache Temporal Arteritis
Symptom Description Likely Causes Dizziness Light-headedness, vague unsteadiness Orthostatic hypotension, anxiety, arrhythmias , anaemia Vertigo Illusion of movement (rotating/tipping), ± N/V Otolith dysfunction, vestibular neuritis, acoustic neuroma Blackouts Transient loss of consciousness, falls Syncope, seizures, hypoglycaemia , anaemia
Gait Type Features Likely Diagnosis Spastic Gait Jerky, stiff, toe-dragging, narrow base MS, Cerebral Palsy, Bilateral cord lesions Hemiparetic Gait Unilateral circumduction of spastic leg Stroke, Unilateral cord lesion Parkinsonian Gait Short, shuffling steps, stooped posture, difficulty turning Parkinson’s Disease Cerebellar Ataxia Broad-based, unsteady, tremulous Lateral cerebellar lobe disease Truncal Ataxia Unsteady trunk, falls backwards/sideways Midline cerebellar (vermis) lesion Sensory Ataxia High-stepping, stamping, worse with eyes closed (Romberg +ve) Polyneuropathy, Loss of proprioception Slapping Gait Audible foot slap Distal leg weakness (e.g. peroneal palsy) Waddling Gait Difficulty rising, proximal leg weakness Muscular dystrophy, Poliomyelitis Gait Apraxia Small, hesitant steps despite intact motor function Frontal lobe disease
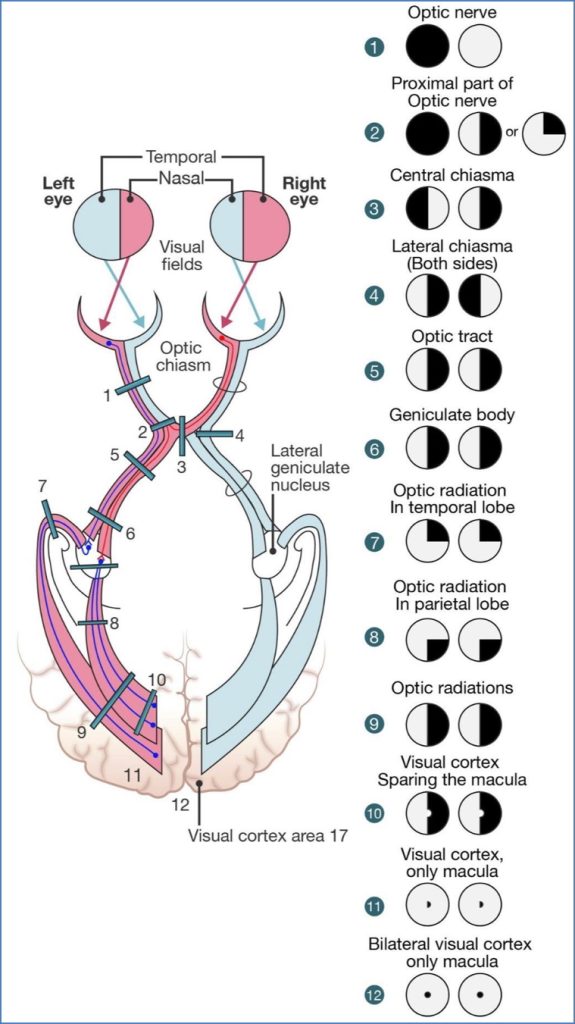
Lesion Location Visual Field Defect Retinal (e.g. haemorrhage) Paracentral Scotoma Optic Nerve (Unilateral)Monocular Field Loss Optic Chiasm Bitemporal Hemianopia Optic Tract (Unilateral) Contralateral Homonymous Hemianopia Parietal Optic Radiation Contralateral Homonymous Upper Quadrantanopia Temporal Optic Radiation Contralateral Homonymous Lower Quadrantanopia Full-Thickness Optic Radiation Contralateral Homonymous Hemianopia Occipital Cortex Contralateral Homonymous Hemiscotoma
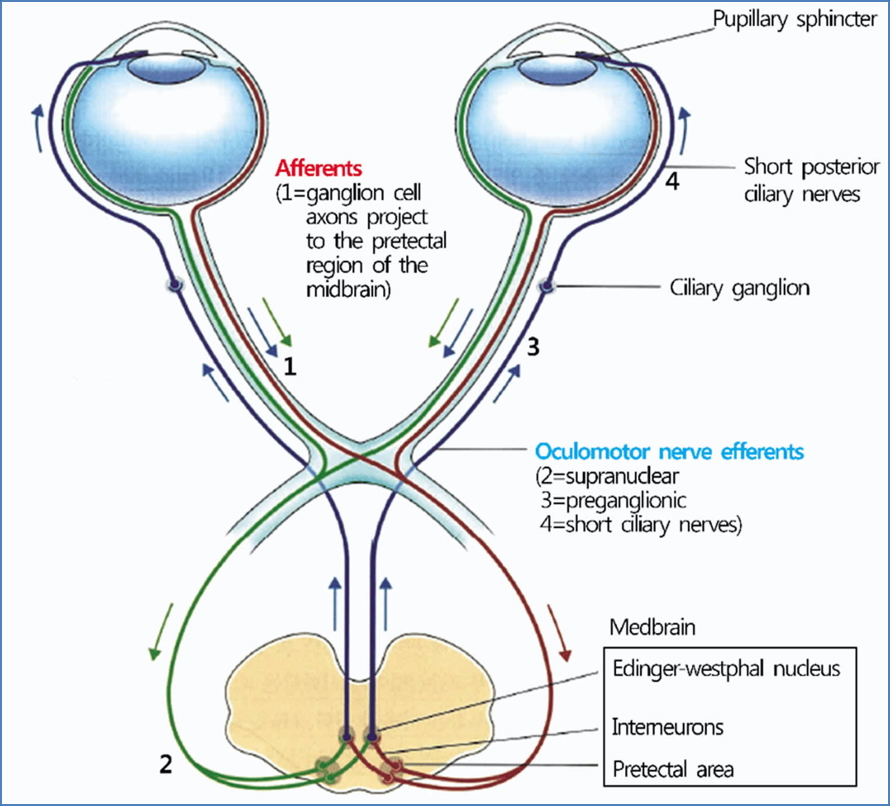
By Urbi Mandal; https://medizzy.com/feed/26426356 Defect Type Key Findings Likely Lesion Site Afferent (e.g. optic nerve) Affected pupil unreactive to light, but consensual reflex present Optic nerve/chiasm/tract Efferent (e.g. CN III palsy) Affected pupil unreactive to light and absent consensual reflex Oculomotor nerve/ciliary ganglion
https://healthjade.net/pupillary-light-reflex/
https://healthjade.net/pupillary-light-reflex/
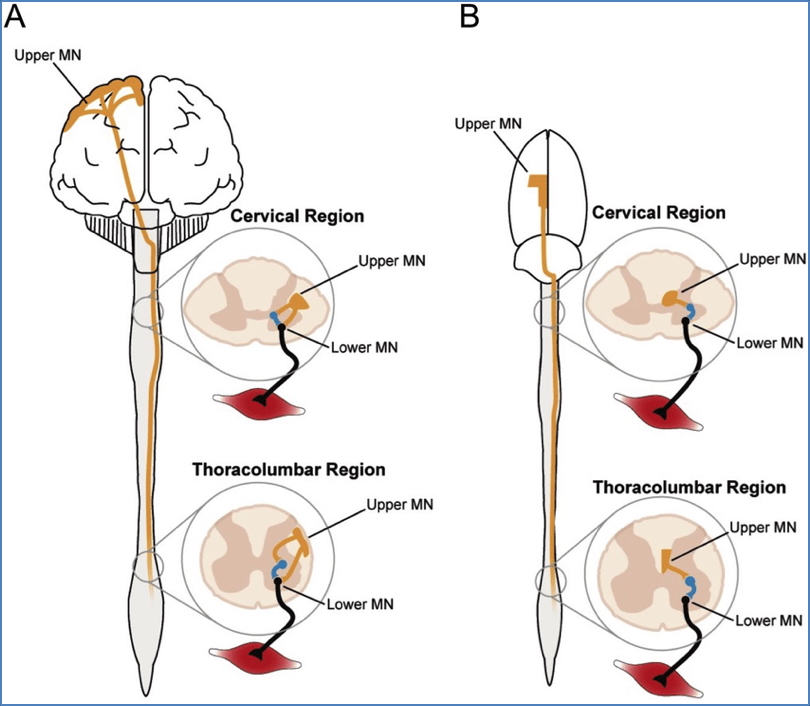
Feature UMN Lesion LMN Lesion Muscle Tone Increased (spasticity) Decreased (flaccid) Reflexes Hyperreflexia Hyporeflexia/Areflexia Muscle Wasting Mild/late Early & severe Fasciculations Absent Present Babinski Sign Present (upgoing toe) Absent Common Causes Stroke, MS, spinal cord injury Peripheral nerve injury, GBS, polio, botulism
Source: Timothy Warner: https://www.researchgate.net/figure/Species-divergent-organisation-of-motor-systems-A-The-corticospinal-tracts-CSTs_fig1_337215634 Pathway Sensation Course Dorsal Column-Medial Lemniscus Vibration, proprioception, 2-point discrimination Ascends ipsilaterally → crosses in medulla Spinothalamic Tract Pain, temperature Crosses at spinal level → ascends contralaterally Trigeminal Pathway Facial sensation Crosses in brainstem Spinocerebellar Tract Unconscious proprioception Stays ipsilateral (mostly), feeds cerebellum
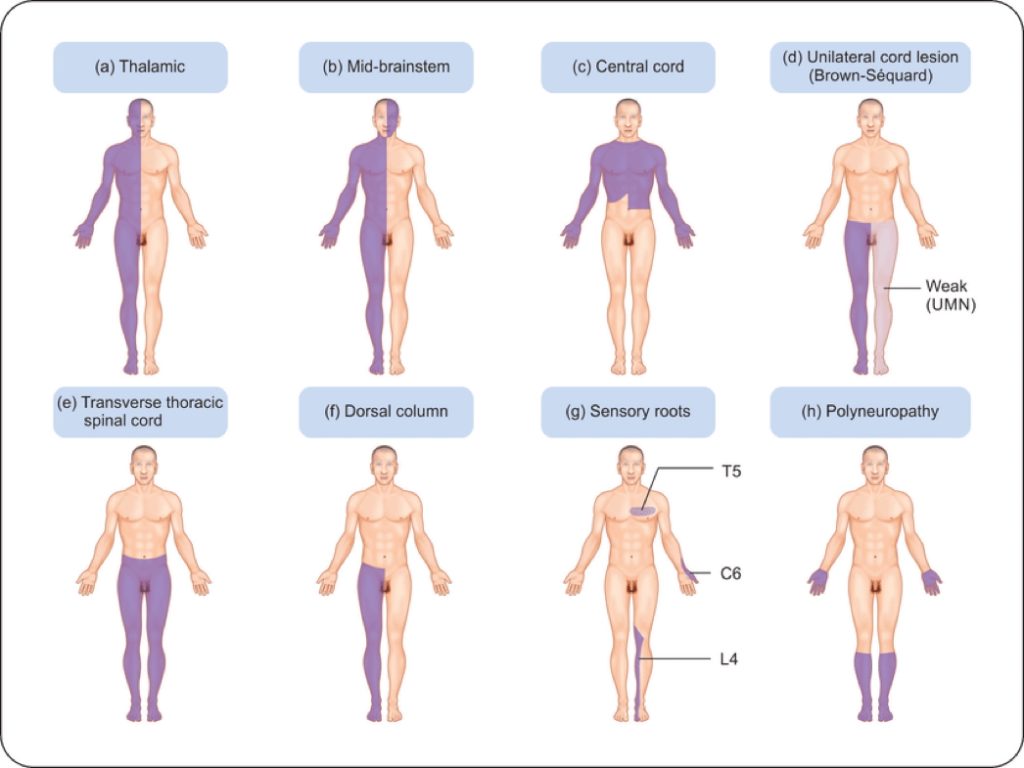
Source: https://www.grepmed.com/images/3568/brownsequard-patterns-loss-diagnosis-bilaterality-neurology-sensory Neurological patterns are high-yield diagnostic tools for identifying the anatomical and pathological source of symptoms such as headaches, blackouts, visual field defects, abnormal gait, or motor/sensory deficits. A structured approach to features like spastic gait, afferent pupillary defects, or Babinski signs helps pinpoint lesions along specific neural pathways. For a broader context, see our Nervous System Overview page.