Table of Contents
Overview – Parkinson’s Disease
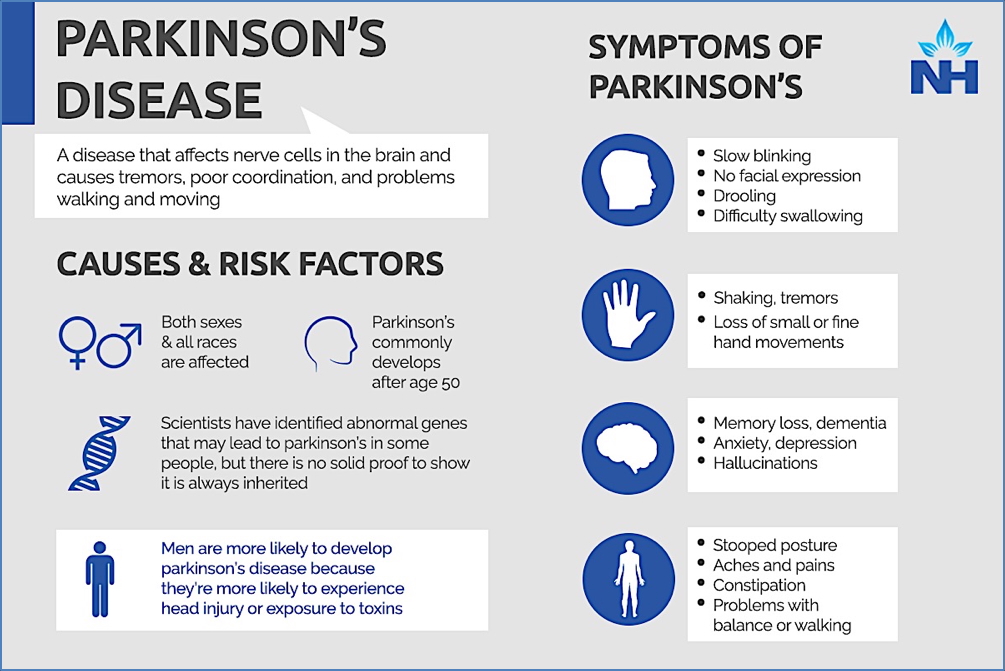
Parkinson’s disease is a progressive neurodegenerative disorder that primarily affects movement due to a loss of dopaminergic neurons in the substantia nigra. This leads to dopamine deficiency in the basal ganglia and subsequent motor dysfunction. It is the second most common neurodegenerative disease after Alzheimer’s. This article explains the clinical presentation, pathophysiology, and treatment of Parkinson’s disease for final-year medical students.
Definition
Parkinson’s disease is an idiopathic neurodegenerative disorder characterised by progressive dopaminergic neuron loss in the substantia nigra, leading to motor dysfunction including tremor, rigidity, and bradykinesia.
Aetiology
- Idiopathic Parkinson’s disease: Primary degeneration of dopaminergic neurons
- Secondary parkinsonism:
- Drugs (e.g. antipsychotics, MPTP)
- Toxins
- Post-encephalitis
- Structural lesions (tumours, strokes)
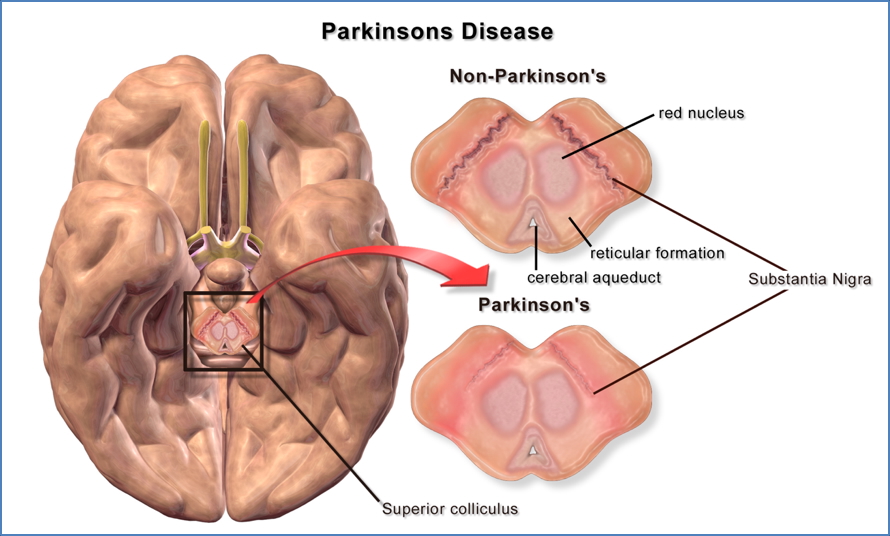
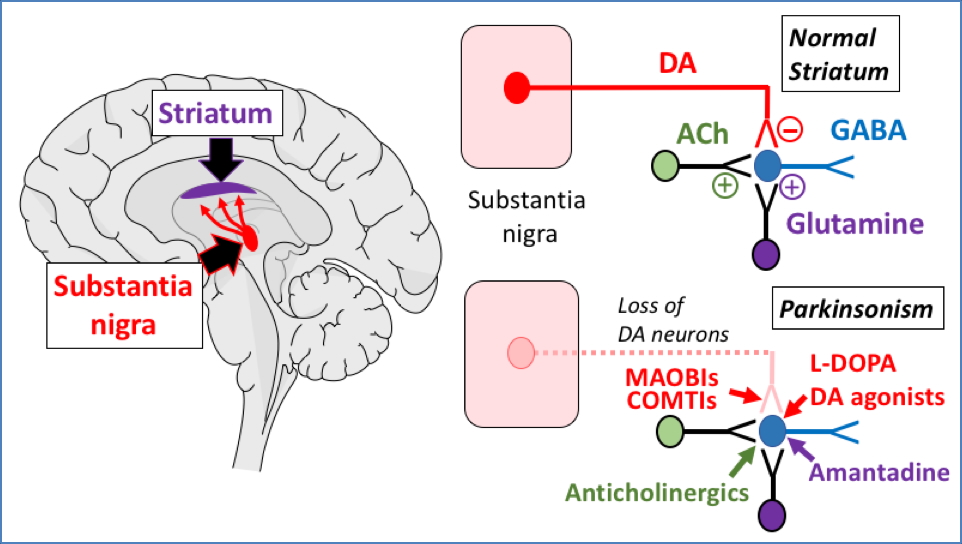
Pathophysiology
- Loss of dopaminergic neurons in the substantia nigra pars compacta
- Results in ↓ dopamine → impaired function of the basal ganglia
- Leads to:
- ↓ inhibition of the globus pallidus
- ↑ inhibition of the ventrolateral thalamus
- ↓ activation of the supplementary motor area (SMA) → impaired movement coordination
- >50% neuron loss required before symptoms appear
- Dopamine imbalance leads to excess ACh activity in the striatum → further contributes to symptoms
Morphology
- Macroscopic: Loss of melanin pigmentation in the substantia nigra
- Microscopic:
- Lewy bodies (α-synuclein aggregates)
- Neuronal loss and gliosis in midbrain structures
Clinical Features
- Triad of Parkinson’s Disease:
- Resting tremor (“pill-rolling” tremor)
- Rigidity:
- Lead-pipe (constant) or cog-wheel (intermittent)
- Bradykinesia:
- Slowness of movement initiation
- Masked facial expression
- Other features:
- Stooped posture
- Shuffling gait
- Hypophonia (soft speech)
- Depression and cognitive decline
- Micrographia (small handwriting)
- Difficulty with fine motor tasks (e.g. doing up buttons)
Investigations
- Clinical diagnosis based on characteristic symptoms
- DaTscan (dopamine transporter SPECT) – helpful in atypical cases
- MRI brain – to exclude secondary causes in young or rapidly progressing cases
Management
Pharmacological
- Levodopa (L-DOPA):
- Crosses the blood–brain barrier and is converted to dopamine
- Given with carbidopa (a peripheral decarboxylase inhibitor)
- Side effects:
- “On-off” phenomenon (fluctuating response)
- Dyskinesias
- Nausea, hypotension
- Dopamine agonists (e.g. pramipexole, ropinirole)
- MAO-B inhibitors (e.g. selegiline)
- COMT inhibitors (e.g. entacapone)
- Anticholinergics (e.g. benztropine) – for tremor-dominant cases in younger patients
Surgical
- Deep Brain Stimulation (DBS):
- Targets subthalamic nucleus or globus pallidus interna
- Reduces motor fluctuations and tremor
- Only for carefully selected patients
- Risks include infection, haemorrhage
Supportive
- Physiotherapy & Occupational Therapy
- Speech therapy
- Psychological support
Complications
- Motor fluctuations and dyskinesia (from long-term Levodopa use)
- Falls and mobility issues
- Depression and dementia
- Autonomic dysfunction (orthostatic hypotension, urinary incontinence)
Differential Diagnosis
- Drug-induced parkinsonism
- Multiple system atrophy
- Progressive supranuclear palsy
- Corticobasal degeneration
- Essential tremor
Summary – Parkinson’s Disease
Parkinson’s disease is a progressive neurodegenerative disorder characterised by dopamine deficiency in the basal ganglia due to substantia nigra neuron loss. It presents with bradykinesia, resting tremor, and rigidity. Treatment is symptomatic, using dopamine replacement and adjunct therapies, with surgical options available for refractory cases. For a broader context, see our Nervous System Overview page.