Table of Contents
Overview
Vertigo is a clinical symptom — not a standalone diagnosis — referring to a false sensation of spinning or movement. It commonly arises from dysfunction in the vestibular system (inner ear or CN VIII), and is a frequent complaint in both emergency and primary care settings. This article outlines key causes and distinguishing features, diagnosis and management for final-year medical students.
Definition
- The Illusion of motion (spinning or tilting), usually exacerbated by head movement.
- Distinct from:
- Presyncope (faintness or light-headedness)
- Disequilibrium (unsteadiness)
- Non-specific dizziness
Pathophysiology
- Originates from mismatch or disruption in sensory input between:
- Vestibular system (labyrinth, semicircular canals)
- Visual system
- Proprioception (joint and muscle sensors)
- Key anatomical structures involved:
- Inner ear
- Vestibulocochlear nerve (CN VIII)
- Brainstem and cerebellum
Common Causes
Motion Sickness
- Cause: Sensory mismatch between vestibular and visual cues.
- Presentation: Nausea, dizziness, cold sweats, pallor.
- Triggers: Travel (cars, boats, planes), simulators, VR.
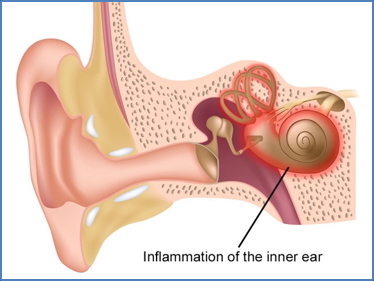
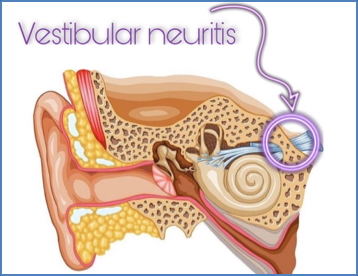
Labyrinthitis & Vestibular Neuritis
- Cause: Viral or bacterial infection; post-viral inflammation; metabolic issues (e.g. hypoglycaemia).
- Distinction:
- Labyrinthitis: Involves both vestibular system and cochlea → vertigo + hearing loss
- Vestibular neuritis: Involves vestibular nerve only → vertigo without hearing loss
- Features:
- Sudden, severe dizziness
- Nausea, vomiting
- Gait imbalance
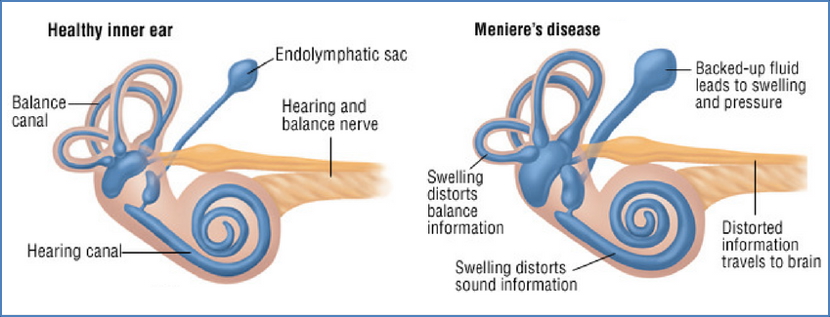
Ménière’s Syndrome
- Cause: Excess endolymphatic fluid → distention of labyrinth
- Features:
- Recurrent episodes (lasting minutes to hours)
- Dizziness, nausea, vomiting
- Tinnitus + fluctuating sensorineural hearing loss
- Triggers: High-salt intake, stress, alcohol
- Diagnosis: Clinical + audiometry
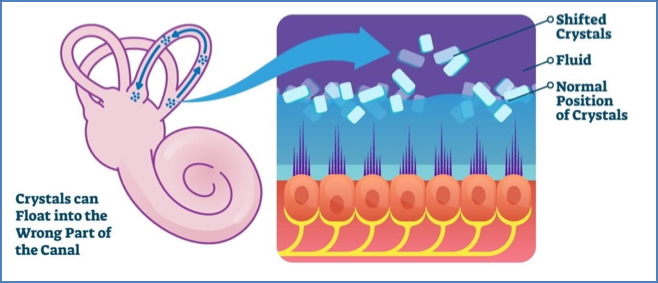
Benign Paroxysmal Positional Vertigo (BPPV)
- Cause: Dislodged otoliths (calcium carbonate crystals) in semicircular canals
- Triggers: Head movements (rolling over, looking up)
- Features:
- Sudden brief episodes (<1 min)
- Vertigo triggered by position changes
- No hearing loss or tinnitus
- Diagnosis: Dix-Hallpike manoeuvre
- Treatment: Epley repositioning manoeuvre
Other Causes
- Drugs: Alcohol, aminoglycosides, anticonvulsants
- Brainstem Lesions: Stroke, multiple sclerosis
- Migraine-associated Vertigo
- Elderly: Vascular insufficiency to inner ear
Investigations
- Clinical manoeuvres: Dix-Hallpike, head impulse test
- Audiometry: Assess for concurrent hearing loss
- Imaging: MRI brainstem/cerebellum if red flags (persistent, focal deficits, ALOC)
- Bloods: Rule out metabolic or infective causes
Management
- BPPV: Epley or Semont manoeuvre
- Ménière’s: Salt restriction, diuretics, betahistine
- Labyrinthitis/Vestibular neuritis: Anti-emetics (prochlorperazine), vestibular rehab
- Motion sickness: Antihistamines (promethazine), scopolamine patches
- Psychogenic vertigo: CBT, SSRIs
Summary
Vertigo is a key symptom indicating vestibular dysfunction, with causes ranging from BPPV and Ménière’s disease to infections like labyrinthitis and neuritis. Accurate history and bedside tests (e.g. Dix-Hallpike) are crucial for diagnosis. For a broader context, see our Nervous System Overview.