Table of Contents
Overview – Breastfeeding and Mastitis
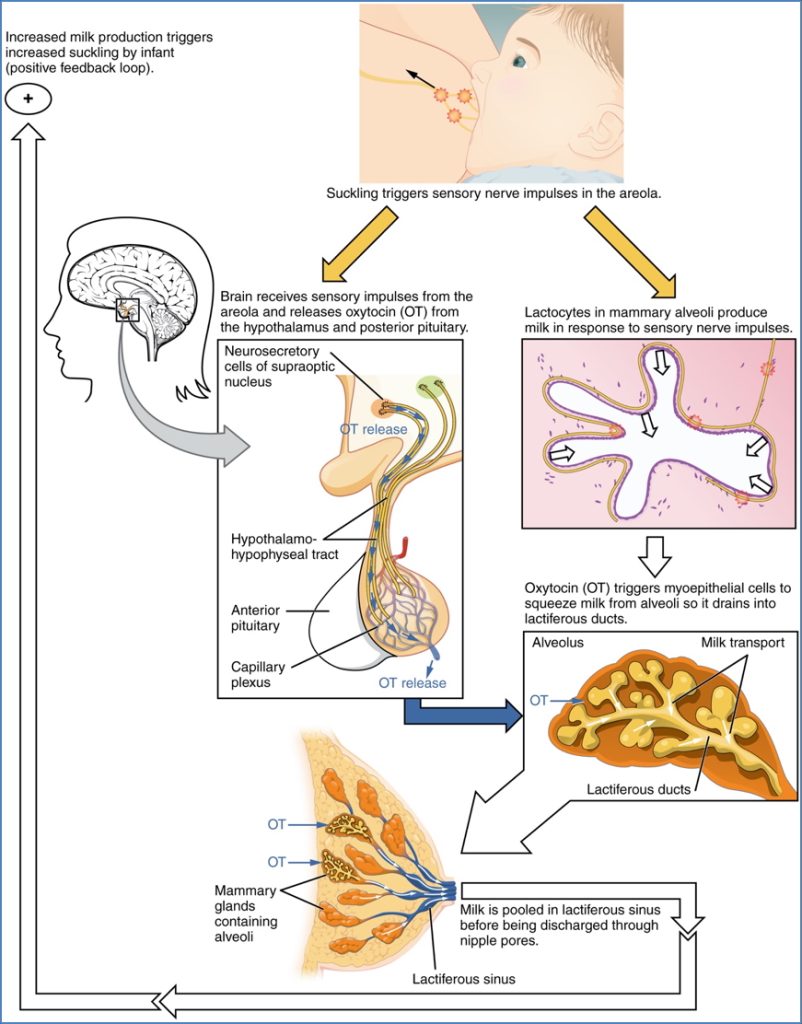
Breastfeeding is a vital component of newborn nutrition, maternal bonding, and postpartum recovery. It is regulated by complex hormonal mechanisms involving prolactin and oxytocin. However, breastfeeding can be complicated by mastitis—an acute inflammatory condition of the breast, usually due to infection. Prompt recognition and management are crucial to reduce maternal discomfort and avoid progression to abscess formation. This article outlines the physiology of lactation and the clinical approach to acute mastitis, making it essential reading for final-year medical students.
Definition
Breastfeeding
- Lactation refers to the production of milk by the mammary glands, typically initiated in late pregnancy and maintained postpartum by infant suckling.
Acute Mastitis
- An inflammatory and/or infectious condition of the breast, usually occurring during the early postpartum period in breastfeeding mothers.
Physiology of Lactation
Hormonal Control
- Late pregnancy:
- High estrogen, progesterone, and human placental lactogen → stimulate hypothalamus
- Hypothalamus releases prolactin-releasing hormone (PRH)
- Anterior pituitary secretes prolactin → milk production
- After birth:
- Mechanical nipple stimulation (infant suckling) maintains prolactin secretion
- Also triggers oxytocin release from posterior pituitary
- Oxytocin → let-down reflex (milk ejection from alveoli)
- Oxytocin also contracts the uterus → aids uterine involution
Colostrum vs Milk
- Colostrum: Secreted in the first 3 days postpartum
- Low lactose and fat
- High in protein, vitamin A, minerals, and IgA antibodies
- Mature milk: Begins production after day 3
Acute Mastitis
Aetiology
- Most commonly caused by Staphylococcus aureus or Streptococcus pyogenes
- Originates from skin flora entering through cracked nipples
- Occurs in 99.9% of cases during lactation, especially early postpartum
Pathogenesis
- Entry of bacteria → local infection → inflammation, pain, erythema
- Can lead to formation of breast abscesses if untreated
Morphology
- Acute inflammatory changes
- Local swelling, erythema
- Purulent discharge or abscess may be present
Clinical Features
- Onset in the first few weeks postpartum
- Unilateral painful, erythematous, swollen breast
- Systemic symptoms: fever, malaise, flu-like symptoms
- Cracked nipples often present
- +/- Purulent discharge
Important Distinction
- Engorgement: Bilateral and non-infective
- Mastitis: Unilateral with systemic signs

Investigations
- Clinical diagnosis is usually sufficient
- Hard, tender, erythematous area of breast + fever in a nursing mother
- Breast ultrasound: To rule out underlying abscess
- Breastmilk culture: Only if severe or hospital-acquired infection
Management
Supportive Care
- Analgesia: Ibuprofen
- Cold compresses to reduce swelling
- Continue breastfeeding (important for drainage)
- Optimise breastfeeding technique:
- Use of nipple shields
- Positioning and latch corrections
Antibiotics
- Empirical anti-staphylococcal agents:
- Cephalexin
- Dicloxacillin
- Clindamycin (if penicillin allergy or MRSA concern)
Summary – Breastfeeding and Mastitis
Breastfeeding is a hormonally regulated process critical to newborn health and maternal recovery. Complications like mastitis—most commonly caused by Staphylococcus aureus—typically occur in the early postpartum period due to nipple trauma and bacterial entry. Prompt diagnosis, continued breastfeeding, supportive care, and antibiotic therapy are key. For a broader context, see our Obstetrics Overview page.