Table of Contents
Overview – Hypertension in Pregnancy
Hypertension in pregnancy refers to elevated blood pressure (≥140/90 mmHg) occurring during or before pregnancy and is a key contributor to maternal and perinatal morbidity and mortality. It can range from chronic hypertension to gestational hypertension, and severe forms like pre-eclampsia and eclampsia. Prompt diagnosis, close monitoring, and appropriate treatment are essential to ensure maternal and fetal safety.
Definition
- Blood pressure ≥140/90 mmHg on two or more separate occasions
- Four clinical classifications:
- Chronic Hypertension:
→ Present before pregnancy or before 20 weeks gestation
→ Associated with increased risk of developing gestational hypertension or pre-eclampsia - Gestational Hypertension:
→ Occurs after 20 weeks gestation
→ No proteinuria or signs of organ dysfunction - Pre-Eclampsia (with or without chronic HTN):
→ Hypertension + signs of maternal organ dysfunction
→ Affects kidneys (proteinuria, raised creatinine), liver (elevated LFTs, RUQ pain), brain (headaches, clonus), hematological system (thrombocytopenia, haemolysis, DIC), or placenta (fetal growth restriction) - Eclampsia:
→ Pre-eclampsia complicated by generalised tonic-clonic seizures
→ Life-threatening emergency requiring urgent intervention
- Chronic Hypertension:
Gestational Hypertension
Risk Factors
- Primigravida (>80% of cases)
- First pregnancy with a new partner
- Diabetes mellitus
- Chronic kidney disease
- Obesity
- Extremes of maternal age (<18 or >35 years)
- Intrauterine growth restriction (IUGR)
- Oligohydramnios
- Multiple gestation
Investigations
- Full clinical exam including BMI and neurological assessment
- Fetal ultrasound and non-stress test
- Bloods: FBC, UECs, LFTs
- 24-hour urine collection (albumin:creatinine ratio)
Management
- Antihypertensives:
- First-line: Labetalol, Nifedipine XR, Methyldopa
- Severe: IV Hydralazine
- Avoid: ACE inhibitors, angiotensin receptor blockers, diuretics, prazosin, atenolol
Complications
- Maternal: renal/liver dysfunction, eclampsia, DIC, HELLP syndrome, stroke, pulmonary oedema
- Fetal: IUGR, prematurity, placental abruption
Pre-Eclampsia and Eclampsia
Aetiology
- Defective placental development and invasion of spiral arterioles
- Risk factors: Primigravida, older maternal age, family history, diabetes, chronic HTN, molar pregnancy, multiple gestation
Pathogenesis
- Placental ischaemia leads to widespread vasoconstriction → hypertension
- Severe disease may result in infarction, multiorgan failure, and seizures (eclampsia)
Clinical Features
- Affects 5–10% of pregnancies
- Symptoms:
- Headaches, visual disturbances
- RUQ/epigastric pain
- Pitting oedema
- Purpura (HELLP syndrome)
- Seizures (eclampsia)
Diagnosis
- Symptom screening: headache, vision changes, oedema, rashes
- BP measurement ≥140/90
- Urine dipstick (proteinuria)
- Blood tests: FBC, UECs, LFTs
- Ultrasound for fetal assessment
Management
- Hospital admission and 4-hourly monitoring
- Serial bloods and fetal USS
- Medications:
- Antenatal corticosteroids (betamethasone)
- Calcium channel blockers (nifedipine), magnesium sulfate infusion
- Beta-blockers (labetalol)
- Definitive management = delivery of the fetus
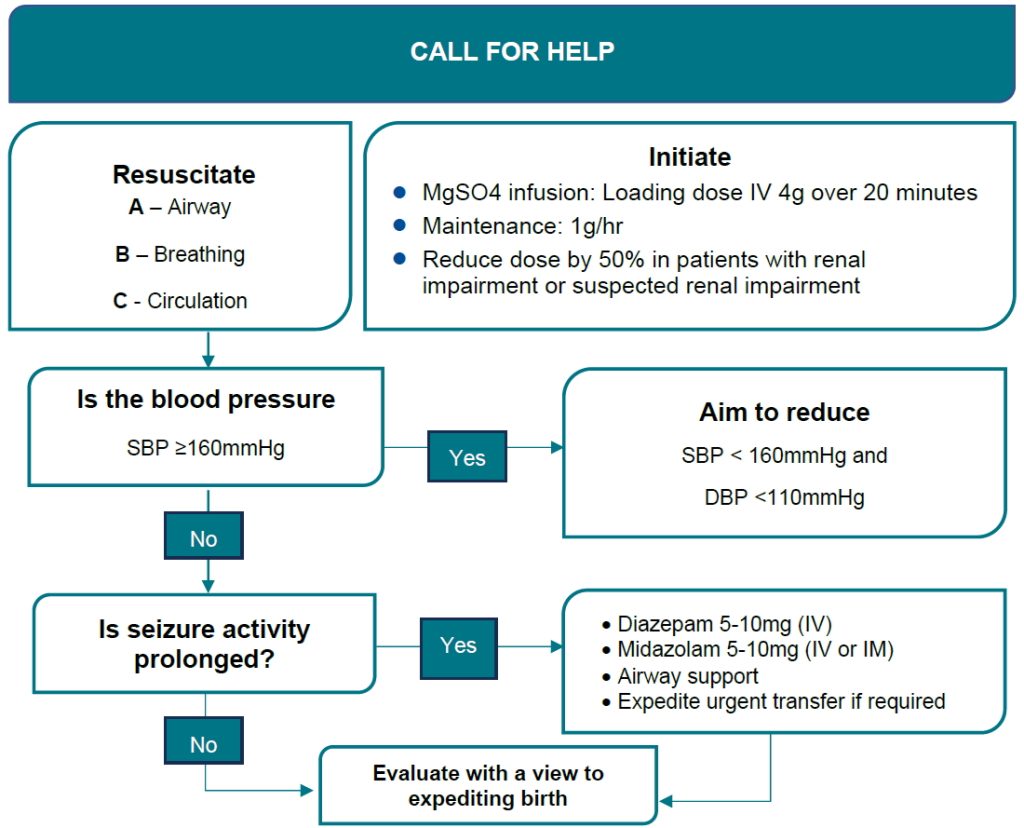
- Eclampsia protocol:
- Stabilise with magnesium sulfate (do not use anticonvulsants)
- Immediate delivery
- ICU/HDU recovery monitoring for ≥4 days post-normalisation of BP
Complications
- IUGR
- HELLP syndrome (haemolysis, elevated liver enzymes, low platelets)
- DIC
- Liver or renal failure
- Placental abruption
- Cerebral haemorrhage
- Aspiration pneumonia
- Death
Prognosis
- Eclampsia is rare with adequate management but carries a ~20% mortality risk if untreated
Summary – Hypertension in Pregnancy
Hypertension in pregnancy includes chronic, gestational, and pre-eclamptic states, all of which carry significant maternal and fetal risks. Pre-eclampsia and eclampsia are severe variants that require urgent management. Early diagnosis, continuous monitoring, and timely delivery are critical. For more, visit our Obstetrics Overview page.