Table of Contents
Overview – Induction of Labour
Induction of Labour (IOL) refers to the artificial initiation of labour prior to its spontaneous onset, with the goal of delivering the fetus when continuing the pregnancy poses greater risks than delivery. It is guided by cervical status, foetal condition, and maternal indications, with careful risk-benefit assessment.
Definition
Induction of Labour = Artificial initiation of labour prior to spontaneous onset, with the intent of delivering the foetus.
Requirements for Induction of Labour
Before performing IOL, the following prerequisites should be met:
- Availability of emergency caesarean section if necessary
- Favourable cervix (short, thin, soft, anterior, dilated os)
- If cervix is unfavourable, consider:
- Prostaglandin vaginal insert
- Misoprostol
- Foley catheter
- Normal foetal heart rate tracing
- Cephalic presentation
- Adequate maternal & foetal monitoring capability
- Bishop Score used to predict likelihood of successful induction:
- <6 = Unfavourable cervix
- ≥6 = Favourable
- ≥9 = High chance of spontaneous vaginal delivery
Bishop Score
Used to assess cervical readiness for labour. Factors scored include:
- Cervical position
- Consistency
- Effacement
- Dilation
- Station
Score Interpretation:
- <5 → Induction unlikely to succeed
- ≥9 → Labour will likely begin spontaneously
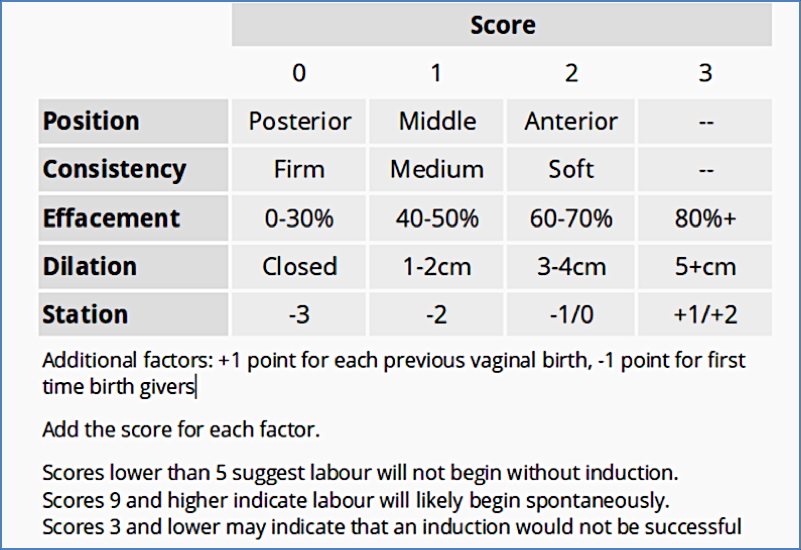
See Bishop Score table above for details
Indications for Induction of Labour
Common clinical scenarios requiring IOL include:
- Post-term pregnancy (>41 weeks)
- Gestational hypertension / Pre-eclampsia
- Maternal diabetes
- Advanced maternal age (>40 years)
- PROM (Premature Rupture of Membranes)
- Chorioamnionitis
- Suspected foetal jeopardy
- Intrauterine foetal demise (IUFD)
- IUGR (Intrauterine Growth Restriction)
- Oligohydramnios or Polyhydramnios
- Multiple gestation (twins)
Contraindications to Induction of Labour
Induction is contraindicated in the following scenarios:
- Prior lower uterine caesarean section or uterine surgery
- Unstable maternal condition
- Active genital herpes infection
- Cervical or uterine anomalies (e.g. cancer, fibroids obstructing the canal)
- Placenta previa / Vasa previa
- Cord presentation
- Malpresentation (e.g. breech)
- Foetal distress or compromise
- Preterm foetus without confirmed lung maturity
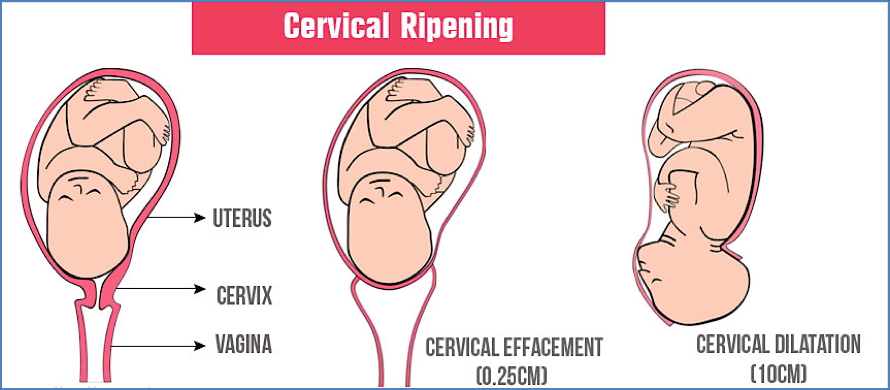
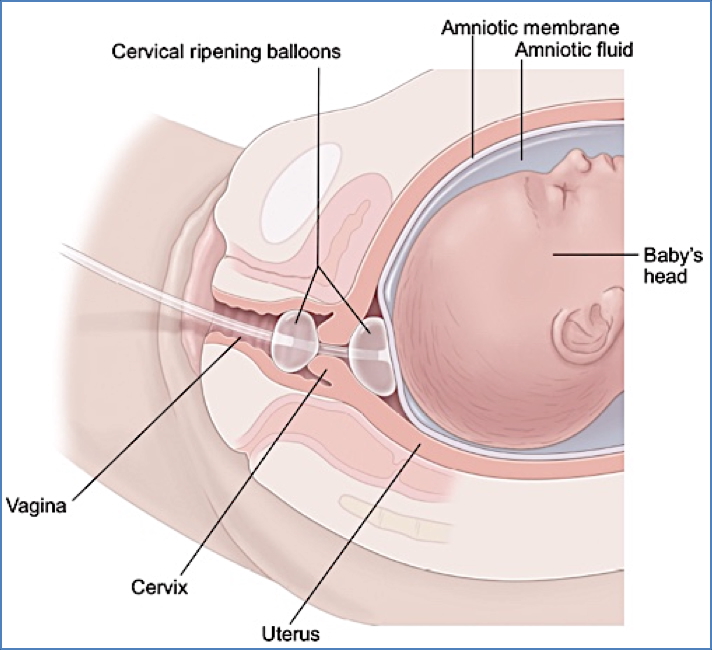
Cervical Ripening
Cervical ripening prepares the cervix for induction by promoting dilation, effacement, and softening.
- Indicated when Bishop Score <6
- Methods:
- Intravaginal prostaglandin gel
- Intravaginal prostaglandin insert
- Intravaginal misoprostol
- Mechanical dilation using Foley catheter
2. https://www.babycenter.com/pregnancy/your-body/inducing-labor_173
Methods of Inducing Labour
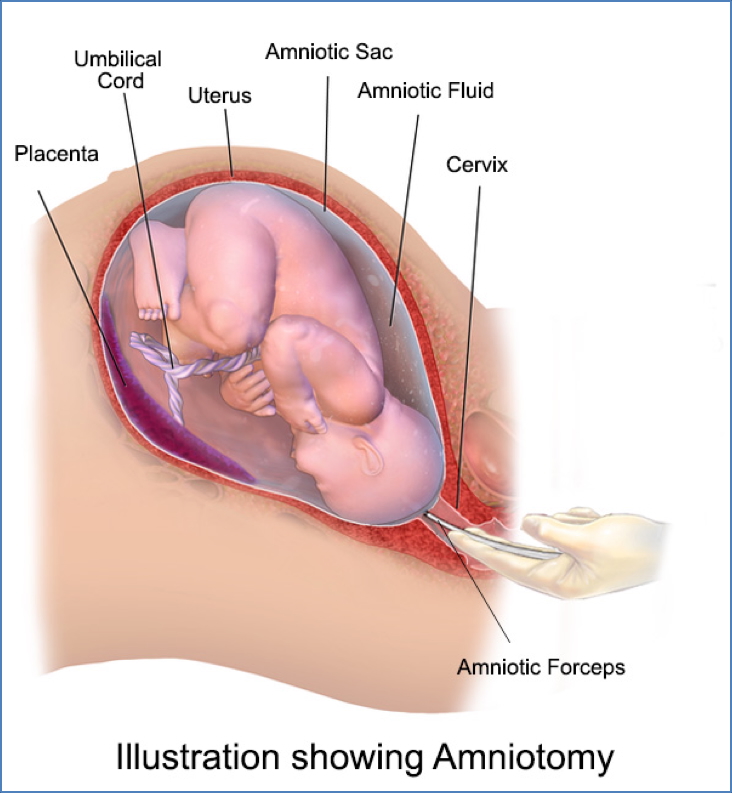
1. Amniotomy
- Artificial rupture of membranes
- Promotes prostaglandin release
- Conditions required:
- Soft, dilated cervix
- Presenting part (usually head) engaged
- Membranes accessible
- Often used in combination with IV oxytocin
2. Oxytocin Infusion
- IV Oxytocin stimulates uterine contractions
- Can reduce rates of failed vaginal delivery
- Risks include:
- Hyperstimulation (uterine tachysystole or tetany) → foetal distress or uterine rupture
- Uterine atony after prolonged use → postpartum haemorrhage (PPH)
Risks Associated with Induction
- Failure to achieve adequate labour or vaginal birth
- Uterine hyperstimulation → Foetal distress or uterine rupture
- Maternal side effects to medications (e.g. GI upset, fever, hypotension)
- Uterine atony → PPH
Summary – Induction of Labour
Induction of labour is a vital obstetric procedure performed when maternal or foetal health may be compromised by prolonging pregnancy. It requires assessment of cervical readiness using the Bishop score and appropriate method selection based on risk factors. With correct application, induction can significantly reduce adverse perinatal outcomes. For more on related obstetric practices, visit our Obstetrics Overview page.