Table of Contents
Overview – Obstetrical Haemorrhage
Obstetrical haemorrhage refers to vaginal bleeding occurring from 20 weeks gestation until term, and is considered a medical emergency. It has multiple potential causes — some benign, some life-threatening — and requires rapid diagnosis and management to reduce maternal and fetal morbidity and mortality. Common causes include placenta previa, placental abruption, and vasa previa.
Definition
- Vaginal bleeding from 20 weeks gestation to term
- Distinguished from earlier bleeding causes such as miscarriage or ectopic pregnancy
Differential Diagnosis
- ‘Bloody show’ – Physiological shedding of the cervical mucous plug before labour
- Placenta previa
- Placental abruption (abruptio placentae)
- Vasa previa
- Cervical lesions – e.g. cervicitis, cervical polyps, ectropion, cervical cancer
- Uterine rupture – Usually in women with previous uterine surgery (e.g. caesarean)
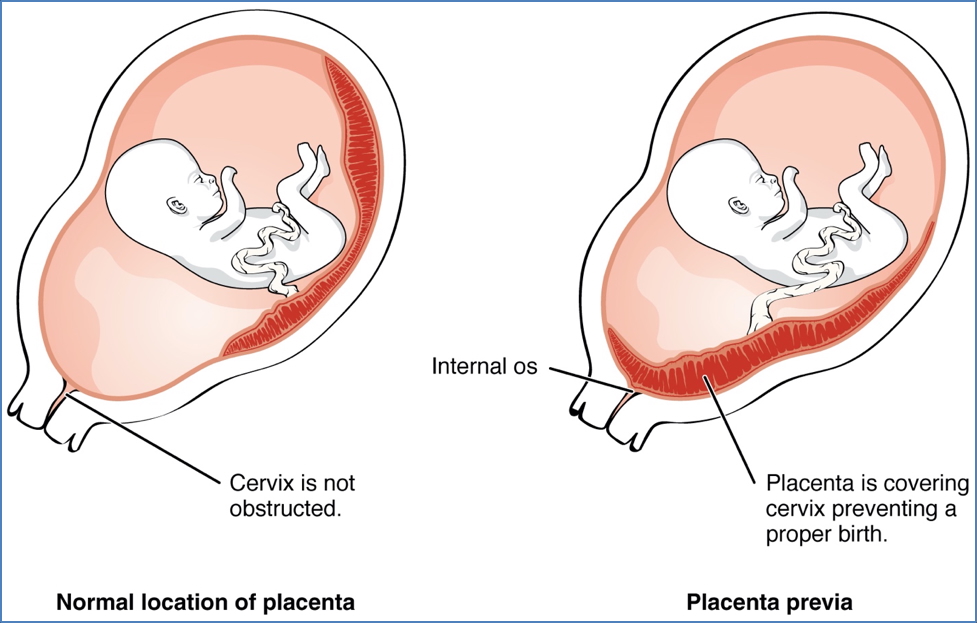
Placenta Previa
Definition
- Placental implantation in the lower uterine segment, over or near the cervical os, ahead of the fetal presenting part
Clinical Features
- Painless, bright red, recurrent vaginal bleeding
- May vary in volume – can be catastrophic
Examination
- Soft, non-tender uterus
- Displaced/high fetal presenting part
- Normal fetal heart rate
Investigations
- Transvaginal ultrasound (TVUS) is the gold standard
- Repeat TVUS in third trimester if placenta is within 20mm of the os at 20 weeks
Complications
- Prematurity due to need for early delivery
- Intrauterine hypoxia
- Malpresentation
- Preterm premature rupture of membranes (PPROM)
- Placenta accreta spectrum
- Maternal risks: anaemia, hypovolaemic shock, Sheehan syndrome, hysterectomy
Management
- Stabilisation: IV fluids, oxygen, and monitor vitals
- Anti-D immunoglobulin if Rh-negative
- If <37 weeks & minimal bleeding:
- Hospital admission
- Corticosteroids for fetal lung maturity
- Limit activity
- If >37 weeks or profuse bleeding:
- Immediate caesarean delivery
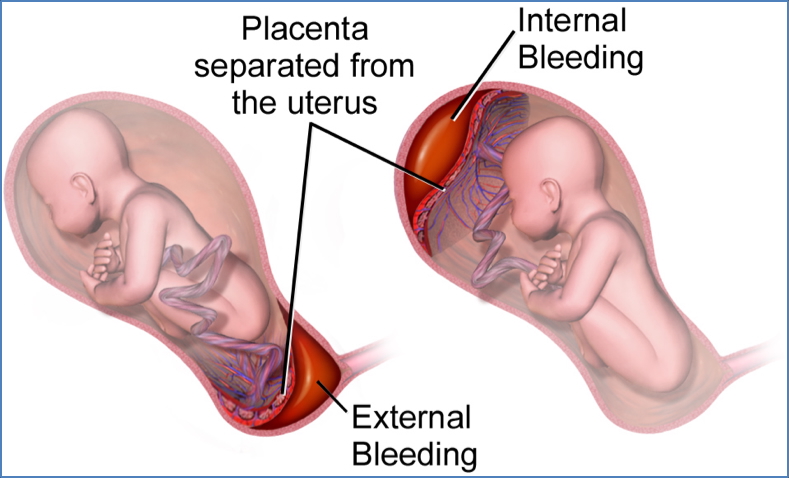
Placental Abruption
Definition
- Premature detachment of the placenta from the uterine wall due to bleeding at the decidual-placental interface
Clinical Features
- Painful, constant, lower abdominal/back pain
- Vaginal bleeding may be absent if concealed abruption
- Uterine tenderness or hypertonicity
- Possible fetal distress or fetal death
Investigations
- Clinical diagnosis
- Imaging is often not sensitive; may assist in ruling out other causes
Complications
- Fetal mortality 25–60%
- Risk of disseminated intravascular coagulation (DIC) ≈ 20%
- Maternal complications: shock, renal failure, Sheehan syndrome, amniotic fluid embolism
Management
- Resuscitation: IV fluids, crossmatch blood, oxygen
- Administer Anti-D if Rh-negative
- Mild abruption:
- <37 weeks: Monitor, consider delivery
- 37 weeks: Stabilise and deliver
- Moderate to severe abruption:
- Vaginal delivery if stable and no fetal distress
- Caesarean if fetal distress or contraindication to labour
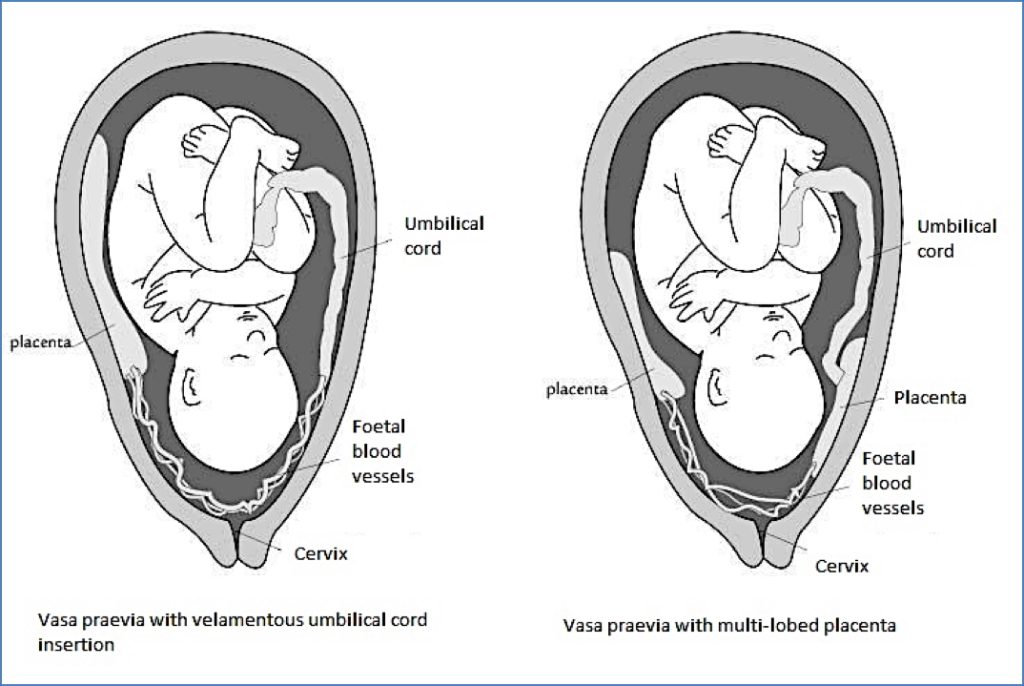
Vasa Previa
Definition
- Fetal vessels traverse the fetal membranes across the internal os, unsupported by cord or placenta
Clinical Features
- Rare (~1 in 5000 pregnancies)
- Increased incidence in multiple gestations
- Painless vaginal bleeding with fetal distress (e.g. sinusoidal CTG pattern)
Investigations
- Apt test: Determines if bleeding is fetal (pink = fetal; yellow = maternal)
- Wright stain: Detects nucleated fetal red cells
Complications
- Fetal mortality ~50% if undiagnosed
Management
- Emergency caesarean section to prevent exsanguination
Summary – Obstetrical Haemorrhage
Obstetrical haemorrhage encompasses life-threatening causes of bleeding after 20 weeks gestation, including placenta previa, placental abruption, and vasa previa. Prompt recognition, investigation, and management are vital to reduce adverse maternal and fetal outcomes. For a broader context, see our Obstetrics Overview page.