Table of Contents
Overview – Postpartum Haemorrhage
Postpartum haemorrhage (PPH) refers to excessive bleeding following childbirth and is one of the leading causes of maternal morbidity and mortality worldwide. While it is more effectively managed in developed settings, PPH remains a major contributor to maternal deaths globally, especially in low-resource environments. Final-year medical students must understand how to promptly recognise, categorise, and manage both primary and secondary PPH to prevent life-threatening complications.
Definition
- Postpartum haemorrhage (PPH) = blood loss >500 mL after childbirth
- Primary PPH = within 24 hours of delivery
- Secondary PPH = between 24 hours to 6–12 weeks post-delivery
Classification by Volume
- Minor PPH: 500–1000 mL blood loss (5–15% of births)
- Major PPH: >1000 mL blood loss (1–3% of births)
Epidemiology & Importance
- Major cause of maternal mortality:
- 1 in 100,000 in Australia
- 1 in 1,000 in developing countries
Pathophysiology
Normal Haemostasis During Delivery
- Myometrial contraction → compresses placental bed
- Pregnancy-induced hypercoagulability (↑ thrombin)
Causes of PPH – “4 Ts”
- Tone: Uterine atony (most common cause)
- Trauma: Perineal, vaginal, or uterine tears; instrumental delivery
- Tissue: Retained products of conception (RPOC)
- Thrombin: Coagulopathies (e.g. DIC, bleeding disorders)
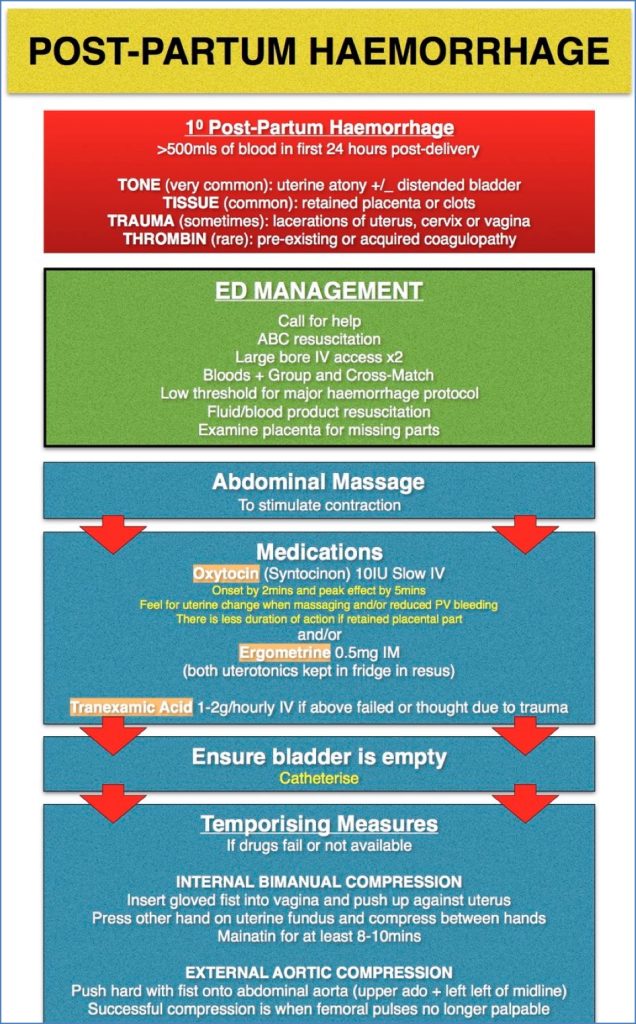
General Management
- Airway, breathing, circulation (ABC) + Call for help
- Insert 2 large-bore IV cannulas → rapid IV crystalloids
- Bloods: Full blood count, coagulation profile, blood group & cross-match
- Catheter for urine output monitoring
- Identify and treat underlying cause
Medical Therapy
- Oxytocin IV
- Ergotamine
- Carboprost (synthetic prostaglandin F2α analogue)
- Misoprostol
- Tranexamic acid
Complications
- Hypovolaemia and shock
- Multiorgan failure (renal, hepatic)
- Sheehan’s syndrome (postpartum pituitary infarction)
- Acute respiratory distress syndrome (ARDS)
- Disseminated intravascular coagulation (DIC)
- Death
Prevention
- Risk factor screening
- Secure IV access and cross-match on standby
- Administer uterotonic agents (e.g. syntocinon, syntometrin, ergometrin) during the third stage of labour
- Active management of the third stage reduces risk by twofold
- Remember: “An intact, empty and contracted uterus will not bleed”
- If ongoing haemorrhage after one resuscitation attempt → Take to theatre
Primary Postpartum Haemorrhage
Risk Factors
Intrapartum:
- Prolonged labour (→ uterine fatigue)
- Instrumental or caesarean delivery
- Uterine trauma or dystocia
- Tocolytics (↓ uterine contractility)
Postpartum:
- History of PPH
- Bleeding disorders / anticoagulation
- Multiparity, multiple gestation, polyhydramnios, macrosomia
- Chorioamnionitis
- Placental abnormalities (accreta, praevia, abruption)
- Retained products of conception (RPOC)
Management
Minor PPH (500–1000 mL)
- Assess and resuscitate (1x large bore IVC, crystalloids)
- Call for help (registrar or consultant)
- Bloods: Group & hold, cross-match, FBC, rhesus status
- Administer uterotonics (e.g. syntocinon)
- Uterine massage to expel clots
- Manual removal of RPOC
- Bimanual uterine compression if necessary
- Treat underlying cause
Major PPH (>1000 mL)
- All of the above, plus:
- Notify theatre and anaesthetist
- Insert a second large bore IVC
- Insert indwelling catheter
- Administer additional uterotonics
- Transfuse as needed:
- Packed red cells
- Fresh frozen plasma (FFP)
- Cryoprecipitate
- Surgical intervention as needed:
- Balloon tamponade
- B-Lynch suture
- Uterine artery ligation
- Hysterectomy
(Note: Please follow your local therapeutic guidelines)
Goals of Treatment
- Stop the bleeding:
- Uterotonics (e.g. oxytocin, ergometrin, misoprostol)
- Bimanual compression
- Surgical options if needed
- Replace blood loss:
- PRBCs, FFP, cryoprecipitate, platelets, Factor VII
- Close monitoring (ICU):
- Blood pressure
- Urine output
Secondary Postpartum Haemorrhage
Timing
- Occurs >24 hours to 6–12 weeks postpartum
Causes
- Infection (endometritis)
- Retained products of conception (RPOC)
- Gestational trophoblastic disease (rare):
- Molar pregnancy
- Invasive trophoblastic disease
- Choriocarcinoma
- Placental site tumour
Presentation
- Typically slow, continuous bleeding (“trickle”)
Management
- Antibiotics for infection
- Uterine curettage for RPOC
- β-hCG testing (to rule out gestational trophoblastic disease)
- Pelvic ultrasound scan
Summary – Postpartum Haemorrhage
Postpartum haemorrhage is a major obstetric emergency and a leading global cause of maternal death. Recognising the “4 Ts” (tone, trauma, tissue, thrombin) helps guide treatment. Primary PPH typically occurs within 24 hours post-delivery, while secondary PPH occurs weeks later. Prompt resuscitation, uterotonics, and definitive surgical management are key. For a broader context, see our Obstetrics Overview page.