Table of Contents
Overview – Antiarrhythmic Drugs
Antiarrhythmic drugs are used to treat abnormal heart rhythms by modifying ion channel activity or autonomic tone. Antiarrhythmic drugs are divided into four classes (I–IV) based on their primary mechanism of action, targeting voltage-gated sodium, potassium, calcium channels, or β-adrenergic receptors. Additionally, standalone agents like digoxin, adenosine, and atropine are used in specific arrhythmic contexts. These drugs play a central role in restoring normal rhythm, particularly in conditions such as supraventricular tachycardia (SVT), atrial fibrillation (AF), and ventricular tachycardia (VT).
Classification of Antiarrhythmic Drugs
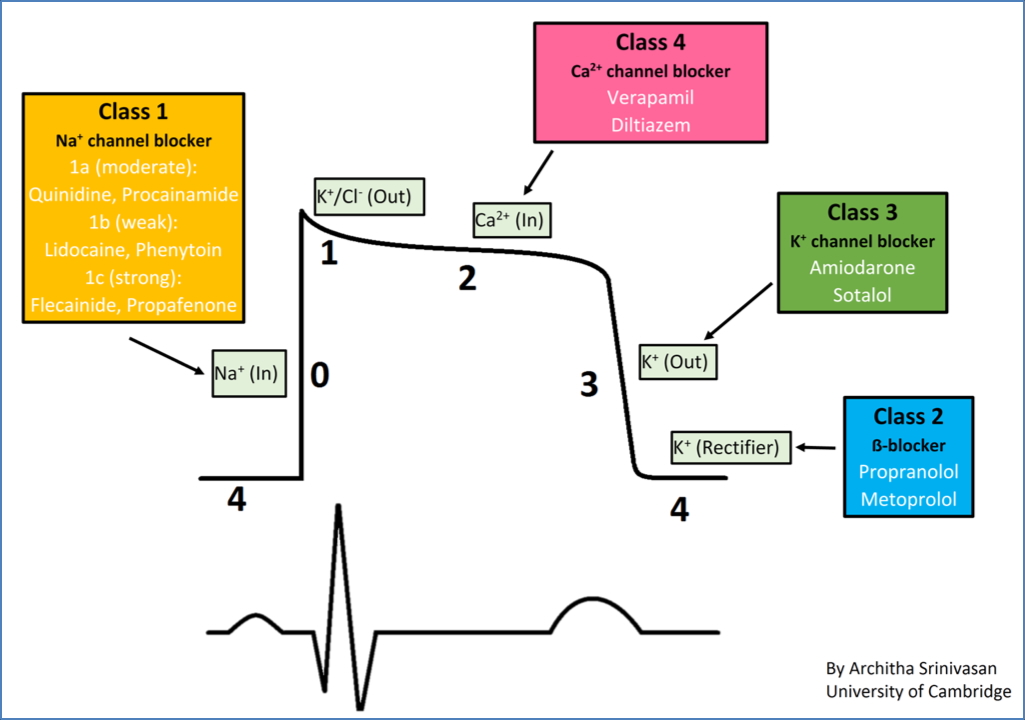
Class I – Voltage-Gated Na⁺ Channel Blockers
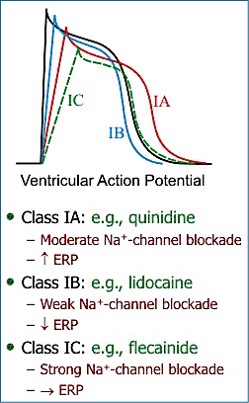
- Mechanism: ↓ Rate of depolarisation in contractile myocytes → ↑ refractory period → ↓ hyperexcitability.
- Use-dependence: Selectively target rapidly depolarising cells (e.g. re-entrant tachycardias) without impairing normal rhythm.
- Subtypes:
- Ia – Quinine, Procainamide: Intermediate association/dissociation; prolongs repolarisation and ↑ AP duration.
- Ib – Lignocaine, Tocainide: Fast kinetics; shortens plateau phase and ↓ AP duration.
- Ic – Flecainide, Encainide, Propafenone: Slow kinetics; markedly ↑ refractory period, minimal effect on AP duration.

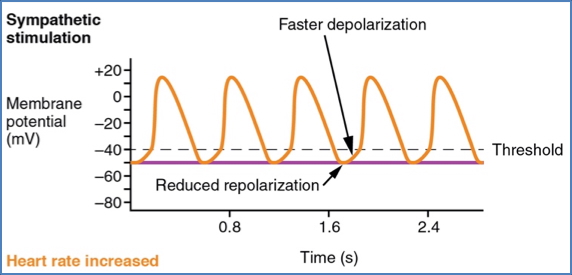
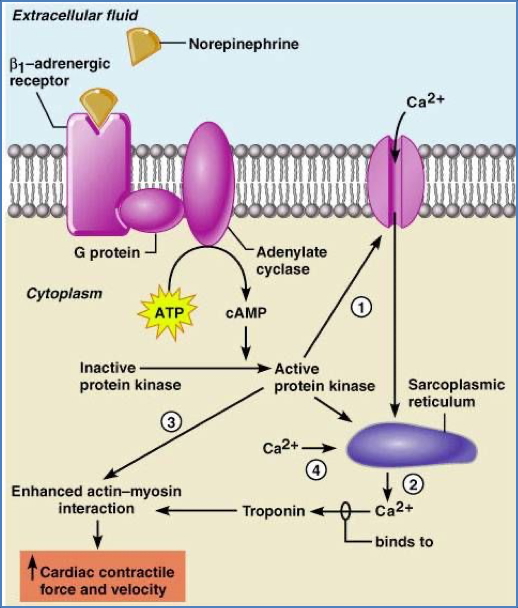
Class II – β-Adrenergic Blockers
- Examples: Propranolol, Esmolol, Atenolol, Pindolol (Note: Sotalol also has Class III action)
- Mechanism: Block β1 receptors → ↓ sympathetic stimulation → ↓ heart rate & contractility.
- Effects:
- ↓ SA/AV nodal activity via reduced Na⁺ and Ca²⁺ permeability.
- ↓ contractility via ↓ intracellular Ca²⁺ in myocytes.
- Indications: AF, SVT, angina, hypertension.
- Contraindications: Asthma (bronchospasm), concurrent Ca²⁺ channel blockers.
- Side Effects: Bradycardia, bronchospasm, rebound tachycardia if withdrawn abruptly.
2. Effects on Contractile Cells: https://www.austincc.edu/apreview/PhysText/Cardiac.html
Class III – Voltage-Gated K⁺ Channel Blockers
- Examples: Amiodarone, Sotalol, Bretylium, Procainamide
- Mechanism: Block VG-K⁺ channels → prolong plateau phase → ↑ refractory period and AP duration.
- Use: Re-entrant tachycardias, VT, AF/flutter.
- Side Effects:
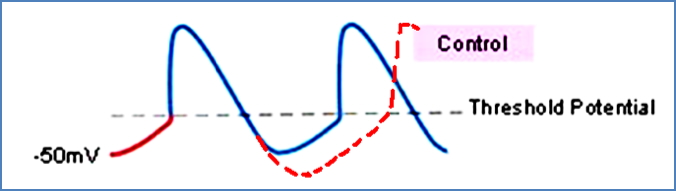
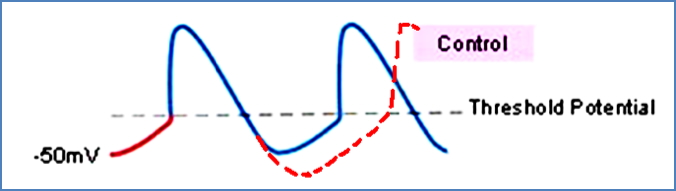
- Early afterdepolarisations (due to AP prolongation).
- Receptor promiscuity (Na⁺ channel and β-blocking effects).

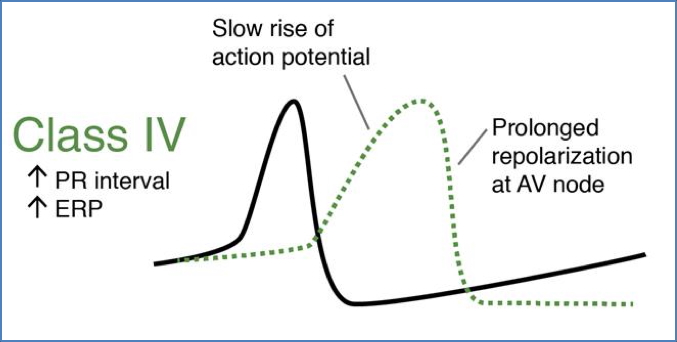
Class IV – Voltage-Gated Ca²⁺ Channel Blockers
- Examples: Verapamil (cardioselective), Nifedipine (vasoselective)
- Mechanism (heart): Block VG-Ca²⁺ channels in SA/AV nodes → ↓ nodal depolarisation → ↓ HR.
- Mechanism (vessels): Block VG-Ca²⁺ in smooth muscle → vasodilation → ↑ coronary supply.
- Use: SVT, angina (especially variant).
- Contraindications: Concurrent β-blocker use → fatal bradycardia risk.
- Side Effects: AV block, bradycardia, hypotension, dizziness.
Detailed Class I Subtypes
Class Ia
- Agents: Quinine, Procainamide
- Kinetics: Intermediate binding/unbinding
- Mechanism: Na⁺ channel blockade → ↑ refractory period; some K⁺ channel blocking → prolongs AP.
- Effect: ↓ hyperexcitability; slows SA node rate.
Class Ib
- Agents: Lidocaine, Tocainide
- Kinetics: Fast binding/unbinding
- Mechanism: Na⁺ channel blockade → ↓ plateau phase → ↓ AP duration
- Effect: Shorter AP but ↑ Na⁺ channel refractoriness (due to delayed recovery).
- Note: Effective for ventricular arrhythmias.
Class Ic
- Agents: Flecainide, Encainide, Propafenone
- Kinetics: Slow binding/unbinding
- Mechanism: Strong Na⁺ blockade → ↑ refractory period without affecting AP duration.
- Effect: Useful for re-entrant arrhythmias; some β-blocking and K⁺ channel effects.
Other Standalone Agents
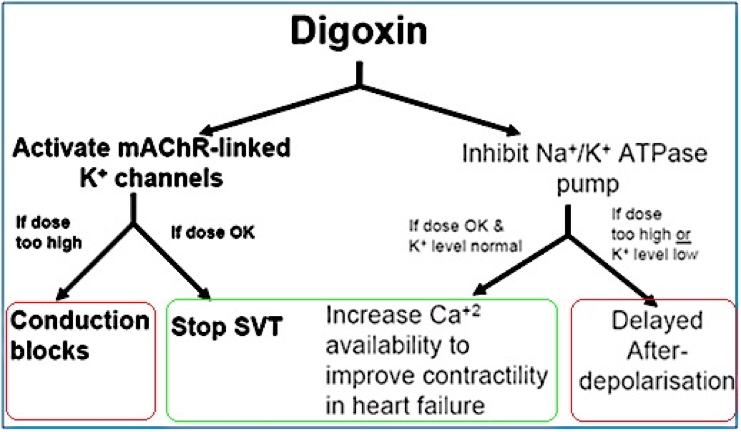
Digoxin
- Use 1: Heart failure (especially with AF)
- Mechanism: Na⁺/K⁺ ATPase inhibition → ↑ intracellular Ca²⁺ → ↑ contractility.
- Risks: ↑ intracellular Na⁺/Ca²⁺ → membrane depolarisation → risk of early afterdepolarisations.

- Use 2: Long-term SVT control (AV node rate control)
- Mechanism: Activates mAChR-linked K⁺ channels → hyperpolarises AV node → ↓ conduction.
- Cautions:
- Avoid if HR <60 bpm.
- Monitor K⁺ levels if on diuretics.
Adenosine
- Use: Diagnostic agent to distinguish SVT vs VT; emergency treatment for SVT.
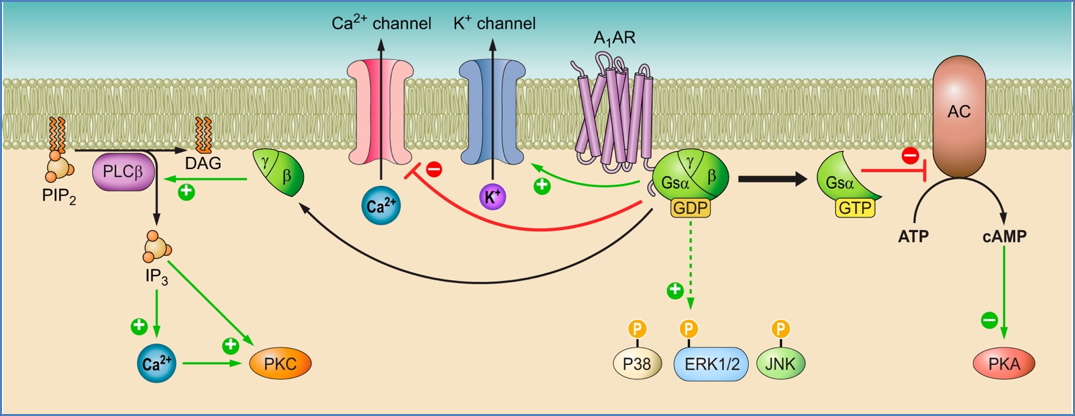
- Mechanism: Binds to adenosine receptors in AV/SA nodes → opens K⁺ channels → hyperpolarises cells → ↓ nodal conduction; also inhibits Ca²⁺ channels.
- Diagnostic role: ↓ HR if SVT; no change in VT.
- Side Effect: Transient chest discomfort or “impending doom”.
Source: https://journals.physiology.org/doi/full/10.1152/physrev.00049.2017
Atropine
- Use: Acute bradycardia or asystole
- Mechanism: M2 muscarinic antagonist → blocks vagal input → ↑ HR.
- Side Effect: High doses may induce VT.

Summary – Antiarrhythmic Drugs
Antiarrhythmic drugs include four main classes (I–IV), each targeting different aspects of cardiac electrophysiology. Class I agents block Na⁺ channels, Class II are β-blockers, Class III block K⁺ channels, and Class IV inhibit Ca²⁺ channels. Standalone agents such as digoxin, adenosine, and atropine provide additional rhythm control in specific clinical contexts. Understanding their mechanisms and risks is essential for the safe management of tachy- and bradyarrhythmias. For a broader context, see our Pharmacology & Toxicology Overview page.