Table of Contents
Overview – Anticoagulant Drugs
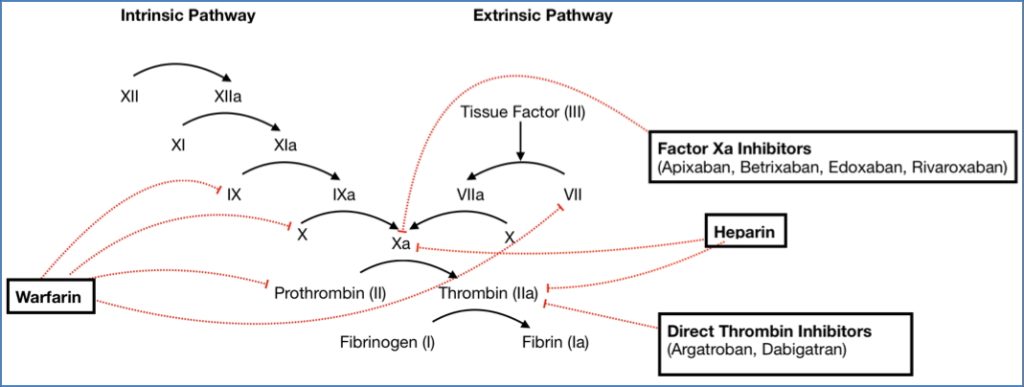
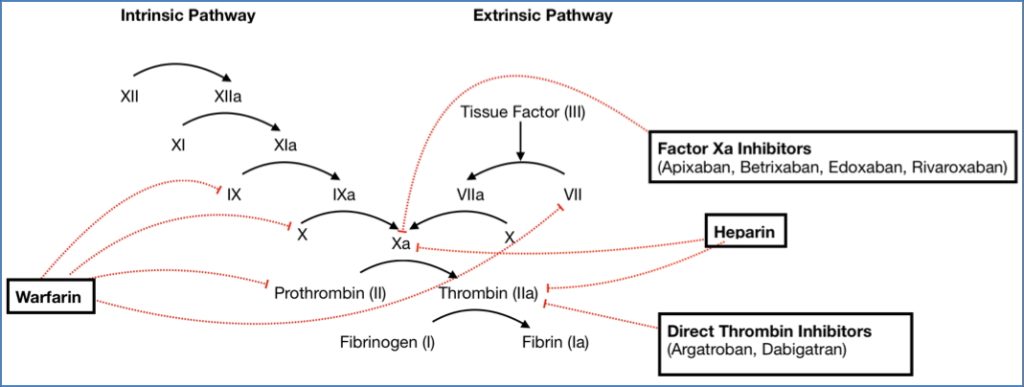
Anticoagulant drugs are a critical part of modern medical therapy, used extensively to prevent and treat thromboembolic conditions. These agents work by interrupting different stages of the coagulation cascade, leading to reduced clot formation. This page focuses on the mechanisms, clinical use, pharmacokinetics, and adverse effects of key anticoagulants including heparin, low molecular-weight heparins, and warfarin, highlighting their differences for safe and effective use.
Heparin
Mechanism of Action
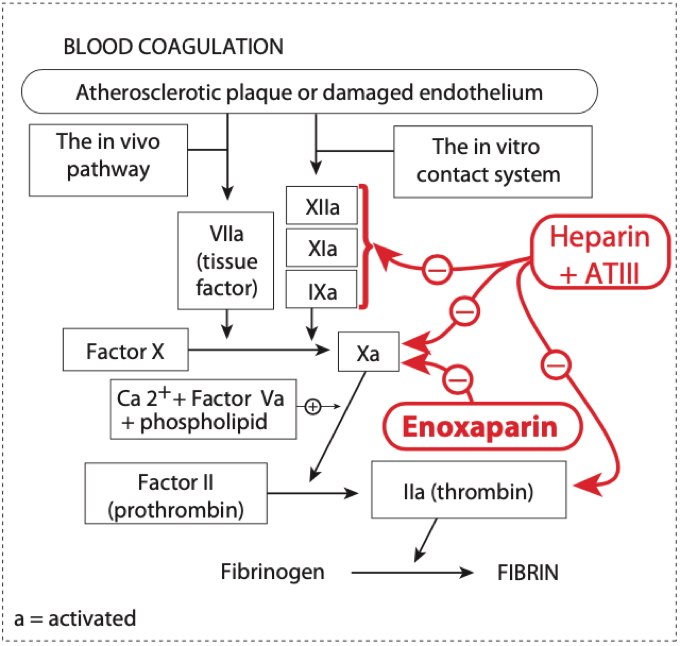
- Binds and activates Antithrombin III (AT-III)
- Heparin–AT-III complex inactivates:
- Thrombin (Factor IIa) → ↓ activation of fibrinogen
- Factor Xa → ↓ conversion of prothrombin to thrombin
- Factors IX, XI, XII → Intrinsic pathway inhibition
Indications
- Acute coronary syndromes (NSTEMI, unstable angina)
- Atrial fibrillation
- Deep vein thrombosis (DVT) and pulmonary embolism (PE)
- Intraoperative and postoperative use in cardiac surgery
Side Effects
- Bleeding
- Antidote = Protamine sulfate
- Heparin-Induced Thrombocytopenia (HIT)
- Type I: non-immune, transient
- Type II: immune-mediated, thrombotic risk
- Others:
- Osteoporosis
- Allergic reactions (e.g. skin necrosis)
- Hyperkalaemia (via hypoaldosteronism)
Pharmacokinetics / Notes
- Rapid onset (IV)
- Not orally bioavailable
- Requires hospital administration and monitoring (aPTT)
Low Molecular-Weight Heparins (LMWHs)
What Are They?
- Smaller fragments of heparin (e.g. enoxaparin)
- Bind to AT-III → selective inhibition of Factor Xa only
- Cannot inactivate thrombin due to small size
Advantages over Unfractionated Heparin
- Longer half-life
- Self-administered via subcutaneous injection
- No routine monitoring required
- Predictable dose-response profile
- Suitable for outpatient use
- More expensive than standard heparin
Adverse Effects
- Lower risk of thrombocytopenia than unfractionated heparin
- Bleeding (less frequent but still possible)
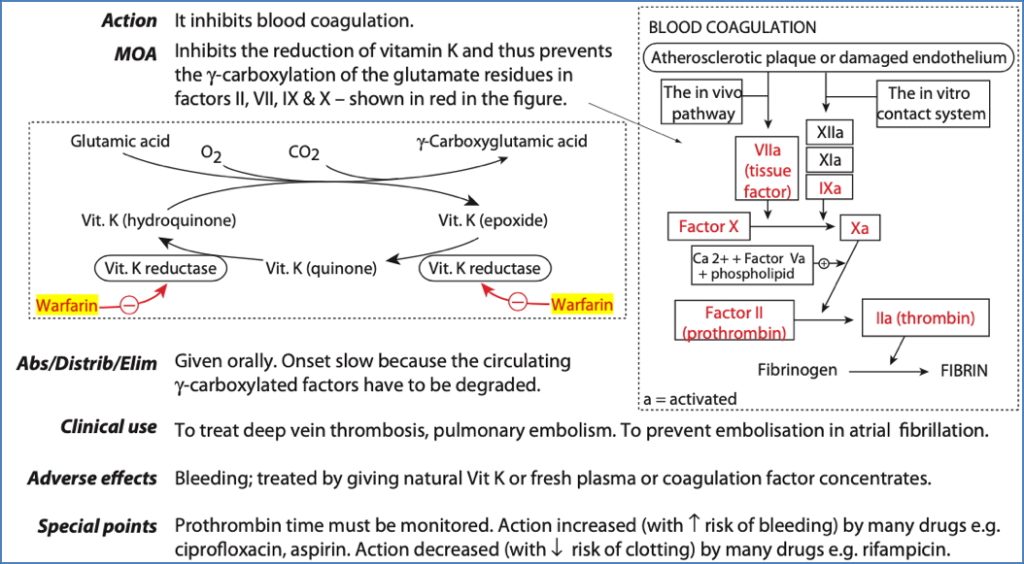
Warfarin
Mechanism of Action
- Vitamin K antagonist
- Competitively inhibits vitamin K epoxide reductase
- ↓ Synthesis of vitamin K-dependent clotting factors:
- Factors II (Thrombin), VII, IX, and X
Indications
- Long-term prevention of:
- Venous thromboembolism
- Atrial fibrillation-associated stroke
- Mechanical heart valve thrombosis
Side Effects
- Bleeding
- Antidote = Vitamin K
- Teratogenic → Contraindicated in pregnancy
- Narrow therapeutic index
- Effectiveness highly variable due to:
- Diet (vitamin K intake)
- Other medications (especially CYP450 inducers like phenytoin, carbamazepine, phenobarbitone)
- Liver function, alcohol use
Pharmacokinetics / Notes
- Slow onset (2–3 days)
- Requires INR monitoring
- Suitable for long-term home use
- Can be reversed with vitamin K or fresh frozen plasma
Heparin-Induced Thrombocytopenia (HIT)
What Is It?
- A reduction in platelet count due to heparin use
Types
- Type I HIT
- Within 1–2 days
- Non-immune, transient, benign
- Type II HIT
- Day 5 onwards
- Immune-mediated (IgG/IgM) against heparin–PF4 complex
- Activates platelets → paradoxical thrombosis despite low platelet count
Summary – Anticoagulant Drugs
Anticoagulant drugs such as heparin, low molecular-weight heparins, and warfarin offer life-saving benefits in the management of thromboembolic disorders. Each class acts at a different point in the coagulation cascade and has unique pharmacological profiles, routes of administration, and monitoring requirements. Understanding these distinctions is vital for safe prescribing and patient safety. For more, see our Pharmacology & Toxicology Overview page.