Table of Contents
Overview – Antiplatelet Drugs
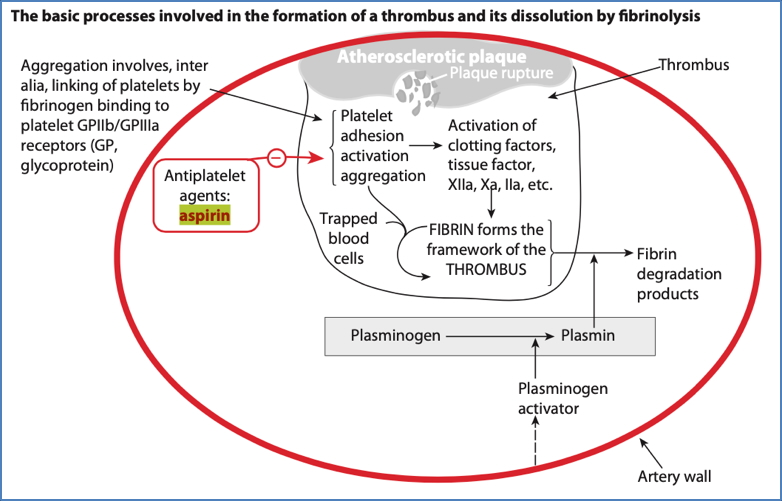
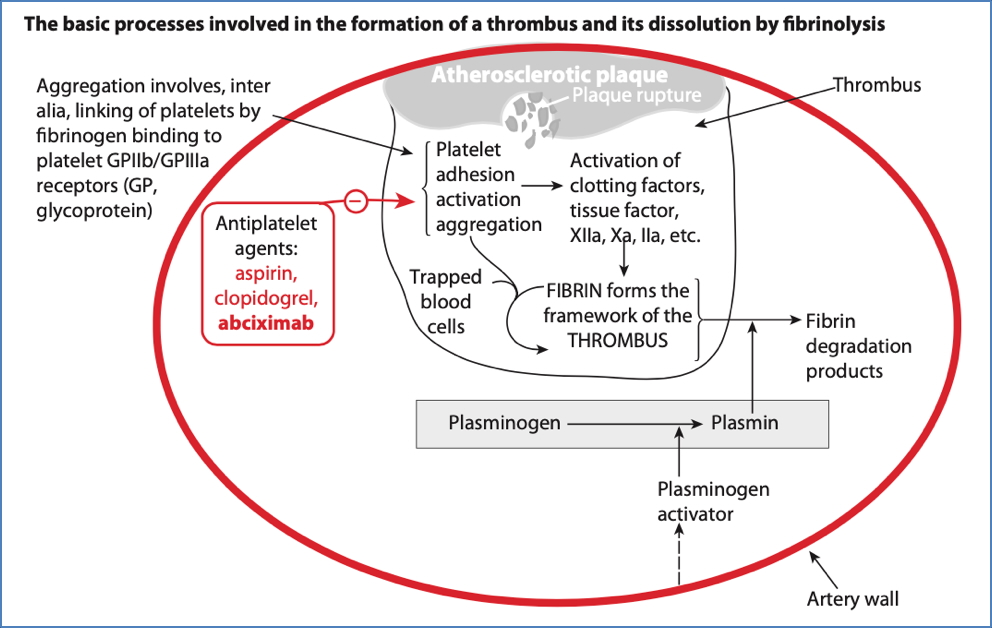
Antiplatelet drugs are essential in the prevention and management of thrombotic cardiovascular and cerebrovascular events. Unlike anticoagulants, which target the coagulation cascade, antiplatelet drugs act on platelet activation and aggregation pathways, reducing arterial thrombus formation. This article outlines the mechanism of action, indications, side effects, and key pharmacological features of major antiplatelet agents including aspirin, dipyridamole, clopidogrel, and abciximab.
Aspirin
Mechanism of Action
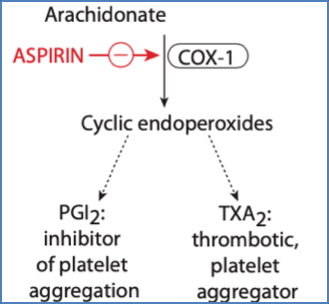
- Irreversibly inhibits Cyclo-Oxygenase-1 (COX-1)
- ↓ Synthesis of thromboxane A₂ (TXA₂), a potent platelet aggregator
- TXA₂ normally activates the GP IIb/IIIa receptor, promoting aggregation
- Platelets lack nuclei → cannot regenerate COX-1
→ Aspirin’s effect persists for the lifespan of the platelet (~7–10 days)
Indications
- Primary and secondary prevention of myocardial infarction (MI)
- Acute ischaemic stroke or transient ischaemic attacks (TIAs)
Side Effects
- Gastrointestinal bleeding (due to ↓ prostaglandins, which normally ↓ acid and ↑ mucus)
- Respiratory alkalosis at toxic doses
Other Information
- Antiplatelet effects occur at low doses (100–300 mg/day)
- Higher doses required for analgesia or anti-inflammatory use (600–5000 mg/day), but now largely obsolete due to GI toxicity
Dipyridamole
Mechanism of Action
- Phosphodiesterase (PDE) inhibitor
- Prevents cAMP breakdown → ↑ cAMP in platelets
- Blocks adenosine reuptake
- ↑ extracellular adenosine → further ↑ cAMP
- ↑ cAMP → ↓ cytosolic calcium →
→ Inhibits calcium-mediated exocytosis of pro-aggregatory granules (e.g., thromboxane)
→ Result = Reduced platelet aggregation
Indications
- Secondary prevention of:
- Ischaemic strokes
- Transient ischaemic attacks (TIAs)
Side Effects
- Headache
- Gastrointestinal upset
- Hypotension
- Allergic reactions
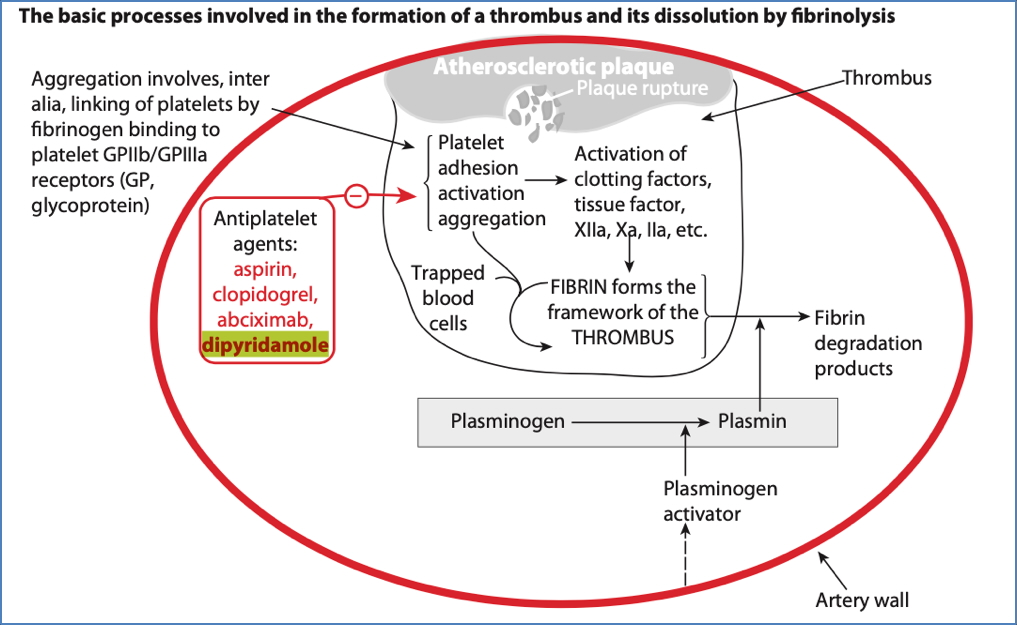
Clopidogrel
Mechanism of Action
- ADP receptor antagonist (P2Y12 receptor)
→ Prevents ADP-mediated activation of GP IIb/IIIa
→ Inhibits platelet aggregation
Indications
- Used in patients intolerant to aspirin
- Often combined with aspirin in dual antiplatelet therapy (DAPT)
- Prevention and treatment of myocardial infarction
Side Effects
- Bleeding
- Gastrointestinal discomfort
- Rash
Other Information
- Prodrug → Requires hepatic activation via CYP450 enzymes
- Onset of effect takes 8–10 days
- Often used with other antithrombotic drugs for synergistic effect
Abciximab
Mechanism of Action
- Monoclonal antibody targeting GP IIb/IIIa receptor on platelets
→ Inhibits final common pathway for platelet aggregation - Also interferes with vitronectin receptors, which mediate cell adhesion during thrombosis
Indications
- Adjunct during angioplasty (percutaneous coronary intervention)
- May be used to prevent thrombus formation during neurovascular surgery
Side Effects
- Bleeding
- Thrombocytopenia
Other Information
- Name derives from its development process (well number + “-mab” for monoclonal antibody)
Summary – Antiplatelet Drugs
Antiplatelet drugs such as aspirin, clopidogrel, dipyridamole, and abciximab form the foundation of arterial thromboembolic prevention, particularly in myocardial infarction and stroke. Each agent targets a distinct mechanism in the platelet activation and aggregation pathway, with varying routes, onset, and risk profiles. Understanding these differences is vital for effective and personalised cardiovascular risk management. For more, see our Pharmacology & Toxicology Overview page.