Table of Contents
Overview – Heart Failure Drugs
Heart failure drugs are used to manage the complex pathophysiology of chronic and acute heart failure, aiming to improve symptoms, reduce hospitalisation, and increase survival. These drugs work by modifying preload, afterload, contractility, and neurohormonal activation to restore effective cardiac output and reduce myocardial strain.
Therapeutic Goals in Heart Failure Management
Management is based on four key targets:
1. Reducing Excessive Preload (Ventricular Filling Pressure)
Lifestyle Modifications:
- Reduce salt and fluid intake → ↓ fluid retention → ↓ central venous pressure → ↓ preload
- Often overlooked but essential in hypertension and heart failure control
Vasodilators:
Organic Nitrates (e.g. Isosorbide Mononitrate – ISMN)
- Exogenous nitric oxide donor
- Activates guanylate cyclase in vascular smooth muscle → ↑cGMP → ↓ intracellular Ca²⁺ → smooth muscle relaxation → vasodilation
- Reduces both preload and afterload

ACE Inhibitors (e.g. Perindopril, Captopril, Enalapril)
- ↓ Angiotensin II → ↓ arteriolar constriction, ↓ salt/water retention, ↓ sympathetic tone
- Ultimately → ↓ central venous pressure → ↓ preload
- Also slows progression of heart failure via neurohormonal blockade

Diuretics:
Amiloride (K⁺-sparing epithelial Na⁺ channel inhibitor)
- Inhibits Na⁺ reabsorption in collecting ducts → ↓ H₂O retention
- Preserves potassium levels
Aldosterone Antagonists (e.g. Spironolactone)
- Block aldosterone-mediated upregulation of Na⁺ channels and TCA enzymes
- ↓ Na⁺ and H₂O reabsorption → ↓ preload
- Also used to prevent cardiac remodelling
2. Reducing Excessive Afterload (Ejection Pressure)
Direct Vasodilators:
- Organic Nitrates: Reduce systemic vascular resistance → ↓ afterload → ↓ myocardial workload
Vaso-Selective Ca²⁺ Channel Blockers:
- e.g. Nifedipine, Amlodipine, Nimodipine
- Block vascular smooth muscle VG-Ca²⁺ channels → vasodilation
- Do not use cardioselective Ca²⁺ blockers as they may reduce contractility

Central Sympathetic Inhibitors:
- Clonidine: Stimulates CNS α₂-adrenoceptors → ↓ noradrenaline outflow → vasodilation
- Avoid peripheral α₂ agonists (which cause vasoconstriction)

Peripheral NA-Release Inhibitors:
- Reserpine: Blocks noradrenaline release → vasodilation via reduced sympathetic tone
3. Enhancing Contractility (Inotropic Support)
Cardiac Glycosides:
Digoxin
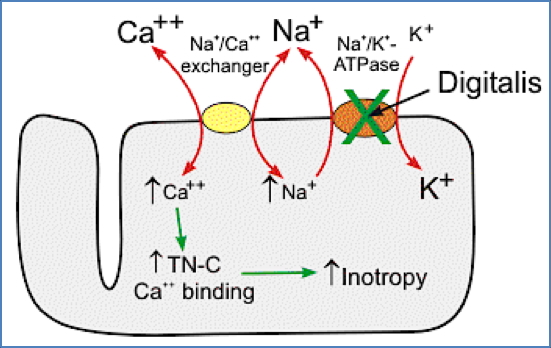
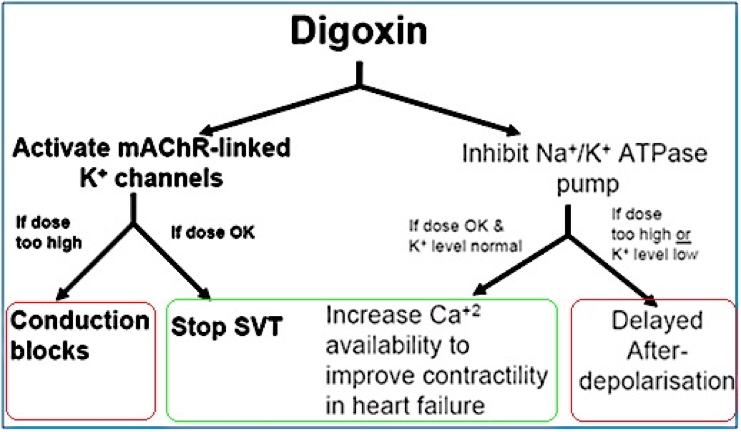
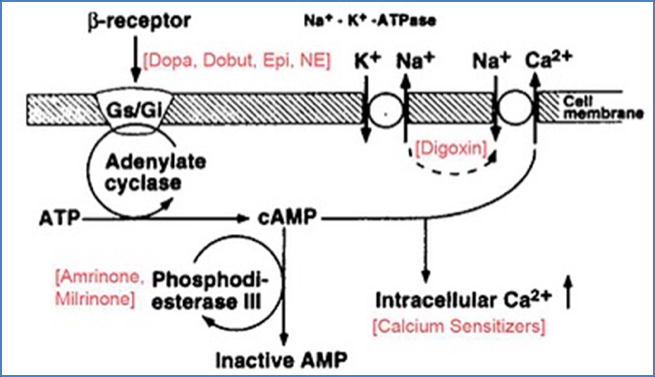
- Inhibits Na⁺/K⁺-ATPase → ↓ Na⁺ efflux → ↑ intracellular Ca²⁺ → improved contractility
- Also slows AV conduction by activating mAChR-linked K⁺ channels
- Monitoring potassium is essential, especially if on K⁺-wasting diuretics
- Risks: Early afterdepolarisations, heart block
β-Adrenergic Agonists:
- Dopamine, Dobutamine
- ↑ cAMP → ↑ intracellular Ca²⁺ → inotropy
- Also improve renal perfusion
- May cause peripheral vasodilation

Phosphodiesterase Inhibitors:
- Milrinone, Amrinone, Vesnarinone
- Inhibit PDE → sustained cAMP/cGMP activity → ↑ Ca²⁺ channel opening → ↑ contractility
- Useful in acute decompensated heart failure
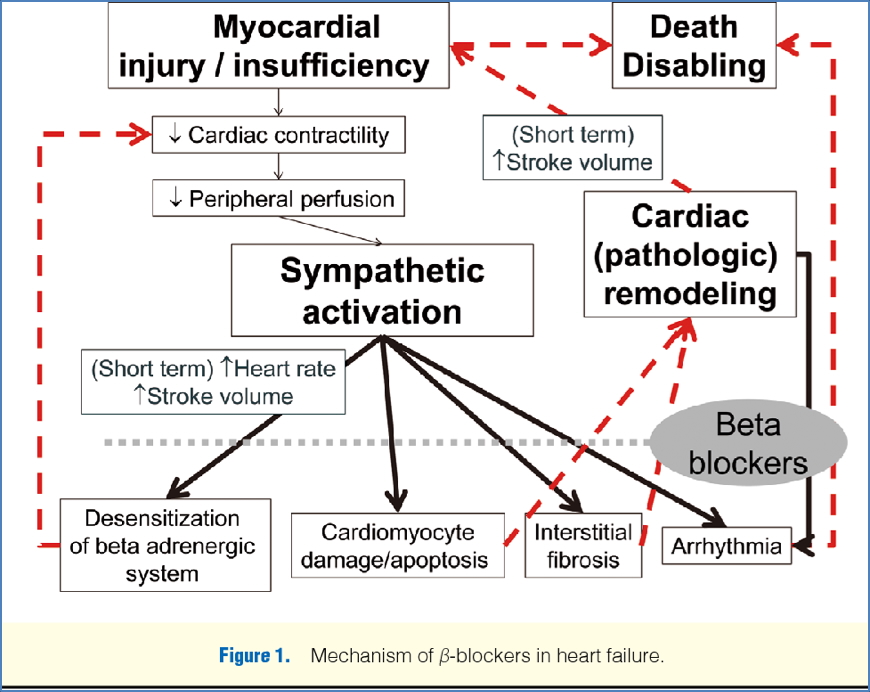
4. β-Blocker Use in Chronic Heart Failure
Specific β-Blockers:
- Carvedilol, Metoprolol, Bisoprolol
- These are inverse agonists, not just antagonists
- ↓ sympathetic drive → facilitate reverse cardiac remodelling:
- ↑ myocyte number
- Alter ion-channel and receptor expression
- Reduce sensitivity to noradrenaline
Only these three β-blockers are indicated in heart failure – others may worsen outcomes.
Summary – Heart Failure Drugs
Heart failure drugs are used to target preload, afterload, contractility, and neurohormonal pathways. They include vasodilators like nitrates and ACE inhibitors, inotropes like digoxin and dopamine, and neurohormonal modulators such as β-blockers and aldosterone antagonists. For a broader context, see our Pharmacology & Toxicology Overview page.