Table of Contents
Overview – Oral Hypoglycaemics
Oral hypoglycaemics are drugs used primarily in the treatment of type 2 diabetes mellitus. They help lower blood glucose levels via various mechanisms, including stimulating insulin secretion, improving insulin sensitivity, and inhibiting intestinal glucose absorption. These agents are ineffective in type 1 diabetes due to the absence of functional pancreatic β-cells.
Definition
Oral hypoglycaemics are non-insulin medications taken by mouth to reduce blood sugar levels in patients with type 2 diabetes mellitus. They are classified based on their primary mechanism of action.
Strategic Drug Categories
Hypoglycaemic Agents – “Secretagogues”
Stimulate insulin release from pancreatic β-cells.
Examples:
- Sulphonylureas
- Meglitinides
Not effective in type 1 diabetes (β-cell absence).
Euglycaemic Agents – “Sensitisers”
Enhance insulin sensitivity and glucose uptake.
Examples:
- Biguanides
- Thiazolidinediones (TZDs)
Gastrointestinal Glucose Absorption Inhibitors
Inhibit carbohydrate digestion enzymes, thereby reducing glucose absorption.
Example:
- Acarbose
Clinical Use
- Type 2 Diabetes Mellitus – As monotherapy or in combination therapy

Mechanisms of Action (Grouped by Class)
Hypoglycaemic Agents – “Secretagogues”
Sulphonylureas
Examples: Glibenclamide, Glipizide
- Stimulate insulin release by activating ATP-dependent K⁺ channels on pancreatic β-cells → ↑ insulin secretion
- Indirectly:
- ↓ hepatic gluconeogenesis
- ↑ peripheral glycolysis
Side Effects:
- Weight gain (via appetite stimulation)
- Hypoglycaemia (especially in elderly due to prolonged action)
- Cardiotoxicity
- GI/liver disturbances
Meglitinides
Examples: Repaglinide, Nateglinide, Mitiglinide
- Similar to sulphonylureas
- Deactivate ATP-dependent K⁺ channels → ↓ K⁺ efflux → Ca²⁺ influx → insulin release
- Shorter half-life; preferred around meals to reduce postprandial glucose spikes

Euglycaemic Agents – “Sensitisers”
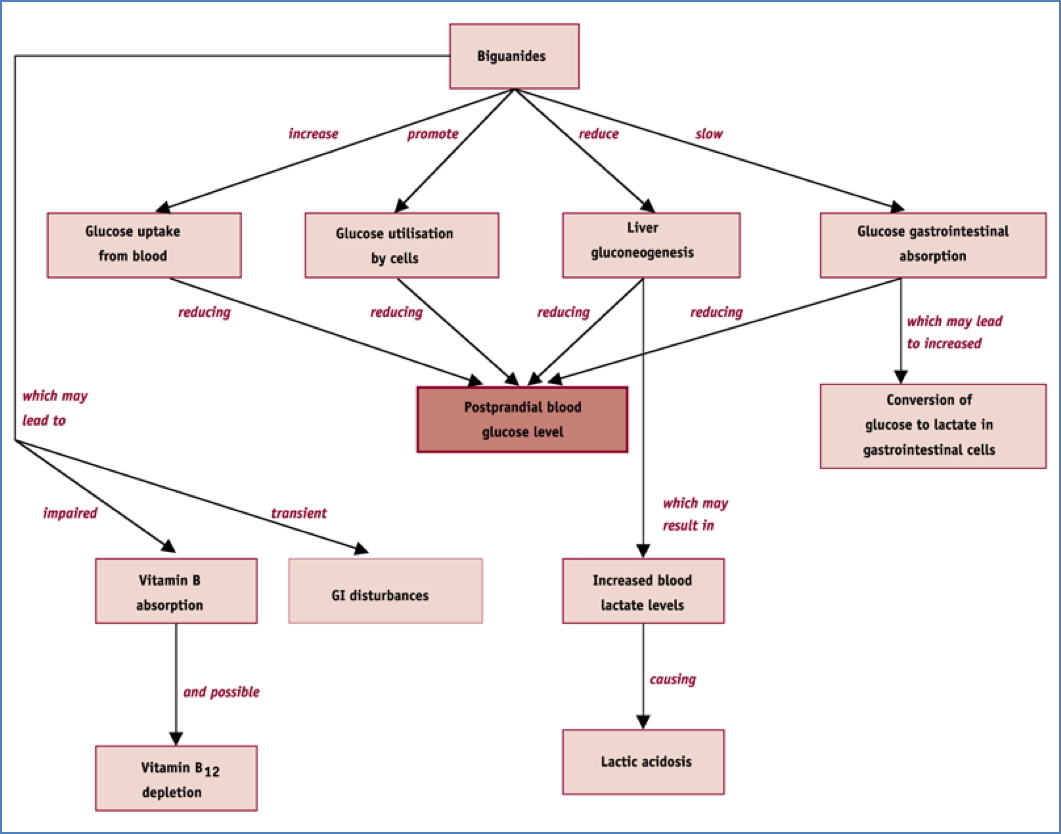
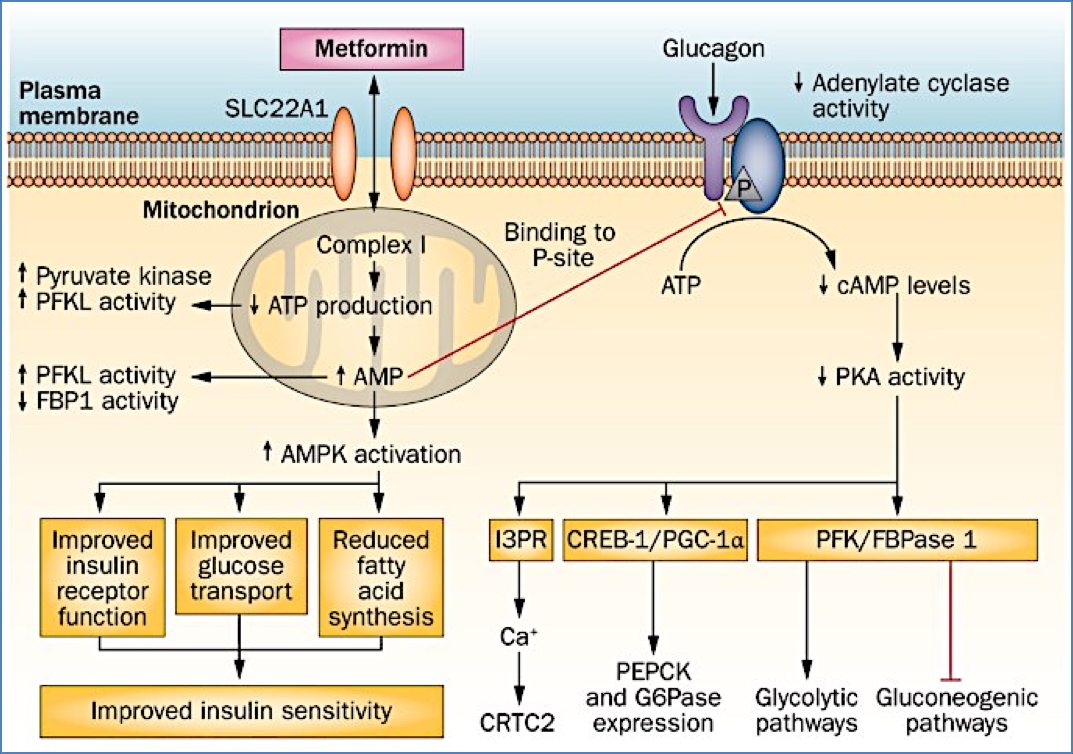
Biguanides
Example: Metformin
- ↓ hepatic glucose output (inhibits gluconeogenesis)
- ↑ peripheral glucose uptake (via enhanced glycolysis)
- Inhibits intestinal glucose absorption
- Minimal risk of hypoglycaemia
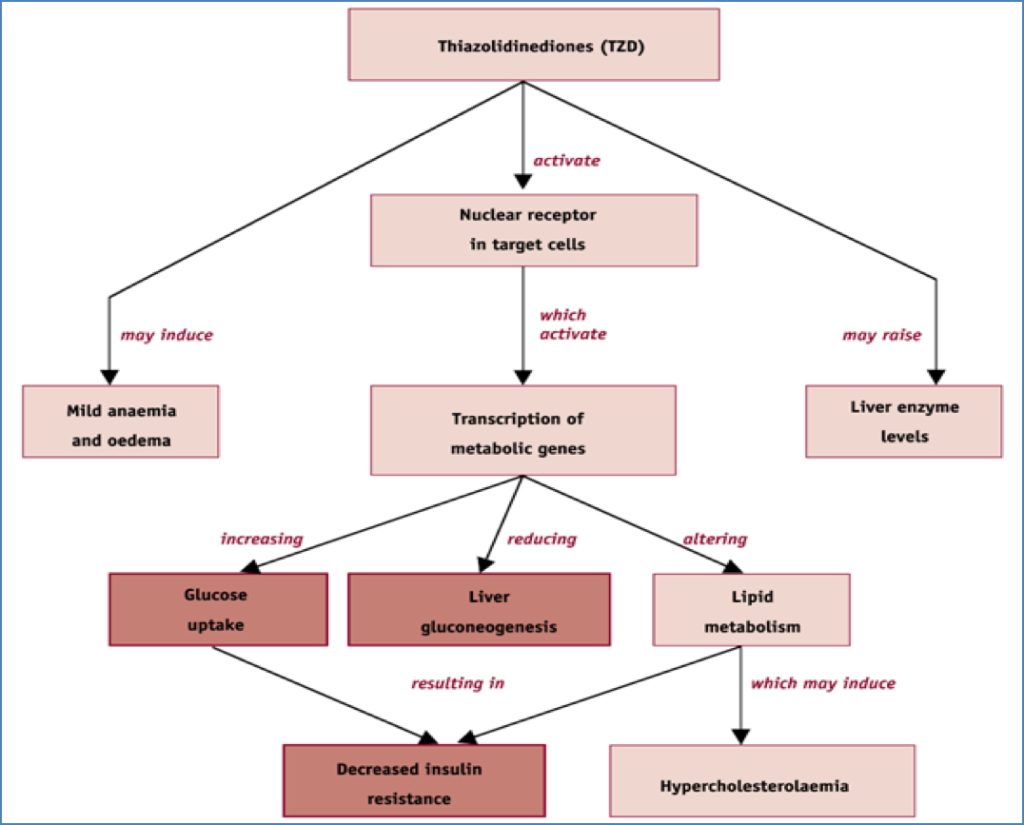
Thiazolidinediones (TZDs)
Example: Rosiglitazone
- Activate nuclear transcription factors (PPAR-γ)
- ↑ transcription of insulin-sensitive enzymes
- ↓ hepatic glucose production
- ↑ peripheral glucose uptake
Gastrointestinal Glucose Absorption Inhibitors
Acarbose
- Inhibits α-glucosidase and amylase → ↓ complex carbohydrate digestion
- ↓ intestinal glucose absorption
- Does not affect monosaccharide absorption
Side Effects: - Flatulence
- Diarrhoea

Summary – Oral Hypoglycaemics
Oral hypoglycaemics are a cornerstone of type 2 diabetes treatment, targeting various pathophysiological mechanisms. These include secretagogues like sulphonylureas, insulin sensitisers like metformin and thiazolidinediones, and carbohydrate digestion inhibitors like acarbose. For a broader context, see our Pharmacology & Toxicology Overview page.