Table of Contents
Overview – Psychology of Pain
Psychology of pain refers to the complex sensory, emotional, and cognitive components that shape how individuals perceive and respond to pain. Pain is not just a physiological response to tissue injury but a deeply personal, subjective experience influenced by biological, psychological, and sociocultural factors. Understanding these dimensions is essential for assessing and managing both acute and chronic pain in clinical practice.
Definition
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage (nociception). It is:
- Subjective and personal
- Modulated by biological, psychological, and cultural influences
- The most common reason people seek medical attention
Unrelieved pain adversely impacts:
- Mood and mental health
- Sleep and cognition
- Appetite and mobility
- Healing capacity and immune response
- Behaviour and overall quality of life
The Cycle of Pain
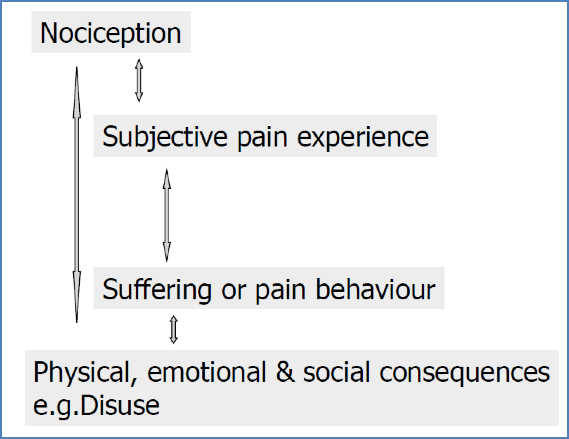
Pain is not linear but cyclical. The model includes:
- Nociception – sensory detection of tissue injury
- Subjective pain experience – perception of pain
- Suffering or pain behaviour – behavioural expression and coping
- Physical, emotional, and social consequences – e.g. immobility, withdrawal, disuse
These stages interact and amplify each other, forming a feedback loop
Factors Influencing the Pain Experience
Biological Factors
- Extent of tissue damage
- Fatigue or comorbid illness
- Presence or absence of analgesia
- Individual health status
Psychological Factors
- Pain threshold and tolerance
- Situational context
- e.g. Distraction during injury can reduce awareness
- e.g. Children may cry more if a parent is present
- Anticipated consequences
- e.g. Suppressing pain to maintain composure in emergencies
Cultural and Social Factors
- Cultural norms (e.g. Stoicism vs expressiveness)
- Religious beliefs (e.g. pain as a test or trial)
- Gender roles and expectations
Psychogenic Pain Disorder
- Clinically significant pain without identifiable physical cause
- Pain causes functional impairment
- Psychological factors play a central role in symptom presentation
Chronic Pain Syndromes
Examples include:
- Chronic low back pain
- Recurrent abdominal pain
- Recurrent tension headaches
- Non-specific musculoskeletal pain (myalgia)
Associated Psychological Syndromes
- Depression
- Anxiety
- Analgesic dependence
Assessment of Pain
Clinical Interview
- How does pain affect the patient’s daily activities?
- What has changed since the pain began?
Assessment Tools
- McGill Pain Questionnaire
- Numeric Rating Scales (e.g. 1–10)
- Mood inventories (e.g. Beck Depression Inventory)
- Self-reported functional impairment
- Behavioural self-monitoring
- Psychiatric evaluation
- Direct observation of pain behaviour
Management of Chronic Pain
Psychological Principles in Therapy
- Express genuine concern and empathy
- Accept negative responses without judgement
- Be patient and persistent
- Clarify the relevance and goals of treatment
- Where appropriate, engage through physical touch (e.g. handshake, hand on shoulder)
Somatic Approaches
- Pharmacological pain relief
- Physiotherapy and physical rehabilitation
- Surgery (when indicated)
Psychological Approaches
- Cognitive-behavioural therapy (CBT) techniques:
- Relaxation training
- Guided imagery or hypnosis
- Distraction and attention diversion
- Contingency management: rewarding functional behaviours
- Treat comorbid depression and anxiety
- Psychodynamic or interpersonal psychotherapy where relevant
Summary – Psychology of Pain
Psychology of pain highlights that pain is more than tissue damage—it’s a subjective, biopsychosocial experience. Chronic pain often involves psychological distress, behavioural adaptations, and social consequences, necessitating a multidisciplinary treatment approach. For a broader context, see our Psychiatry & Mental Health Overview page.