Table of Contents
Overview – Acute Tubular Necrosis
Acute tubular necrosis (ATN) is the most common cause of acute kidney injury (AKI) in hospitalised patients. It results from ischaemic or nephrotoxic injury to the renal tubules, leading to necrosis, tubular obstruction, and reduced glomerular filtration rate (GFR). Clinically, ATN follows a characteristic progression through oliguric, diuretic, and recovery phases. Early identification and supportive care are crucial to prevent progression to irreversible renal damage.
Definition
- Acute tubular necrosis is a form of intrinsic AKI caused by necrosis of tubular epithelial cells, leading to obstruction and loss of renal function.
- It is most often due to ischaemia or nephrotoxins.
Aetiology
- Ischaemic causes:
- Hypoperfusion from shock, heart failure
- Renal artery stenosis
- Malignant hypertension
- Microangiopathies (e.g. HUS)
- Nephrotoxic causes:
- Aminoglycosides (e.g. gentamicin)
- Cisplatin
- Amphotericin B
- NSAIDs
- Lead
- Radiocontrast agents
Pathophysiology
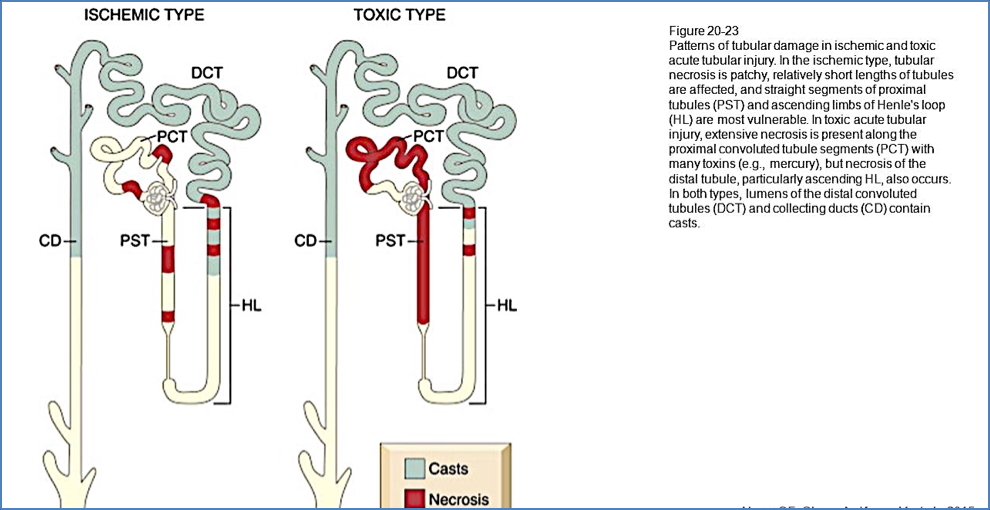
- Ischaemic ATN:
- Poor blood flow → patchy necrosis in proximal tubule and thick ascending limb
- Debris forms casts in distal convoluted tubule (DCT) and collecting duct
- Nephrotoxic ATN:
- Direct toxicity causes uniform necrosis in PCT and descending loop of Henle
- Similar formation of tubular casts in DCT and collecting duct
- Shared downstream effect:
- Tubular obstruction due to sloughed cells
- Increased tubular hydrostatic pressure
- ↓ GFR and ↓ reabsorption → oliguria
- Accumulation of nitrogenous waste → azotaemia
Clinical Features
- Oliguric Phase (7–14 days):
- Low urine output (<400–500 mL/day)
- Rising urea and creatinine
- Diuretic Phase:
- Polyuria (>500 mL/day) as tubules begin recovering
- Risk of volume depletion and electrolyte loss
- Recovery Phase:
- Gradual normalisation of renal function
Investigations
- Renal function tests:
- Elevated urea and creatinine
- Electrolyte abnormalities (e.g. hyperkalaemia)
- Urinalysis:
- Dilute urine
- Muddy brown casts (granular casts of necrotic cells)
- Sometimes biopsy for unclear cases
Management
- Identify and remove the cause:
- Stop nephrotoxic drugs
- Correct hypotension or underlying ischaemia
- Supportive care:
- Fluid and electrolyte management
- Diuretics in fluid overload
- Dietary restrictions:
- Limit sodium, potassium, and fluid intake
- Dialysis:
- Required if refractory fluid overload, hyperkalaemia, or uraemia occurs
Complications
- Prolonged AKI or progression to chronic kidney disease
- Electrolyte disturbances (e.g. hyperkalaemia, acidosis)
- Volume overload
- Infection or sepsis
Differential Diagnosis
- Prerenal AKI (volume depletion, heart failure)
- Glomerulonephritis
- Acute interstitial nephritis
- Obstructive uropathy
- Hepatorenal syndrome
Summary – Acute Tubular Necrosis
Acute tubular necrosis is the leading cause of acute kidney injury in hospitalised patients, resulting from either ischaemia or exposure to nephrotoxins. It follows a stereotypical progression through oliguric, diuretic, and recovery phases. Diagnosis is based on clinical context and characteristic urinary findings, such as muddy brown casts. Supportive care is the mainstay of treatment. For a broader context, see our Renal Overview page.