Table of Contents
Overview – Electrolyte Imbalances
Electrolyte imbalances refer to deviations in the normal concentrations of key ions and solutes in the blood, such as sodium, potassium, calcium, phosphates, and more. These imbalances can significantly disrupt cellular function, neuromuscular excitability, and cardiac rhythm. Medical students must understand the pathophysiology, causes, symptoms, and management of common electrolyte disturbances. This guide provides a structured, high-yield summary of electrolyte and osmolar abnormalities.
Sodium (Na⁺)
Hypernatraemia
- Definition: Elevated serum sodium concentration
- Causes:
- Decreased water intake or increased water loss (reverse-dilution effect)
- Excessive sodium ingestion
- Renal insufficiency
- Effects:
- Cellular dehydration → cell shrinkage
- Hypovolaemia → hypotension → reflex tachycardia
- Intense thirst
- Treatment:
- Rehydration with water
Hyponatraemia
- Definition: Low serum sodium concentration
- Causes:
- Sodium loss (e.g., diarrhoea, sweating, diuretics)
- Excess extracellular water (dilutional)
- Adrenal insufficiency
- Effects:
- Cell swelling → cerebral oedema
- Headache, confusion, seizures, coma
- Treatment:
- Withdraw causative agents (e.g. diuretics)
- Fluid restriction

Potassium (K⁺)
Note: Potassium is essential for repolarisation of excitable membranes.
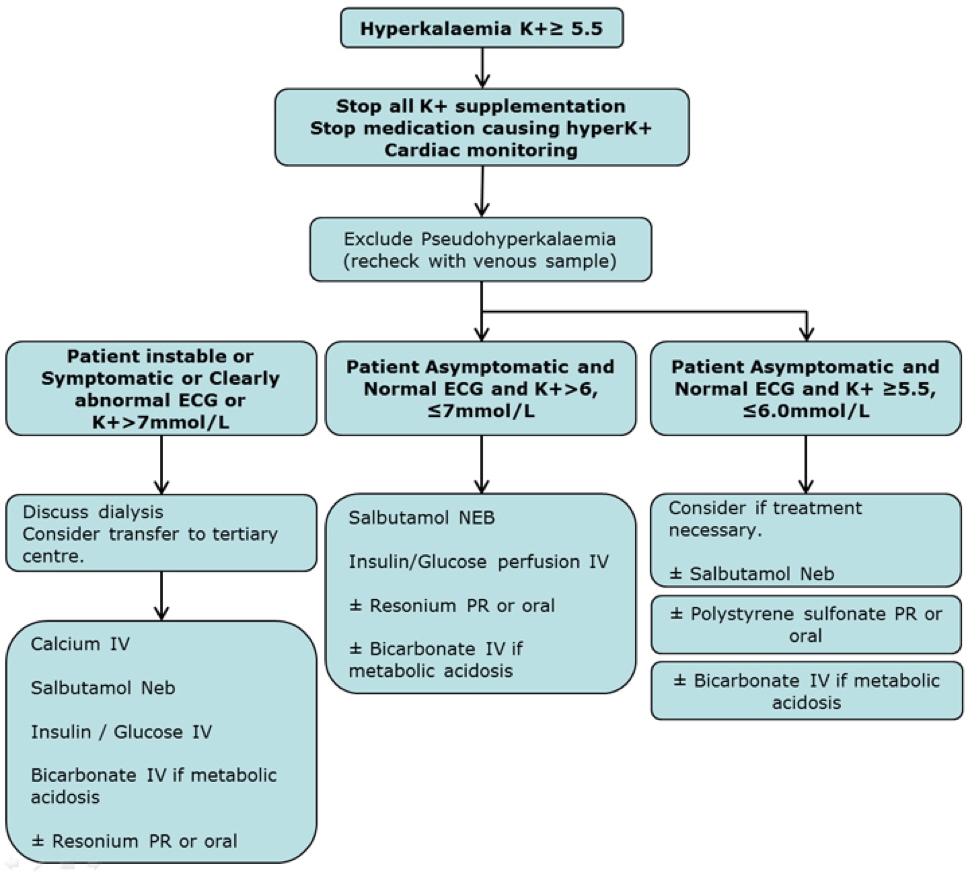
Hyperkalaemia
- Definition: Elevated serum potassium
- Causes:
- Excess intake
- Renal failure (↓ K⁺ excretion)
- Cell lysis from trauma/crush injuries
- Effects:
- Poor repolarisation
- Muscle cramps
- ↓ Cardiac conductivity → risk of arrhythmias
- Treatment:
- Calcium gluconate – stabilises myocardium
- IV insulin – drives K⁺ into cells
- Sodium bicarbonate – activates Na⁺/K⁺-ATPase
- Dialysis in severe cases
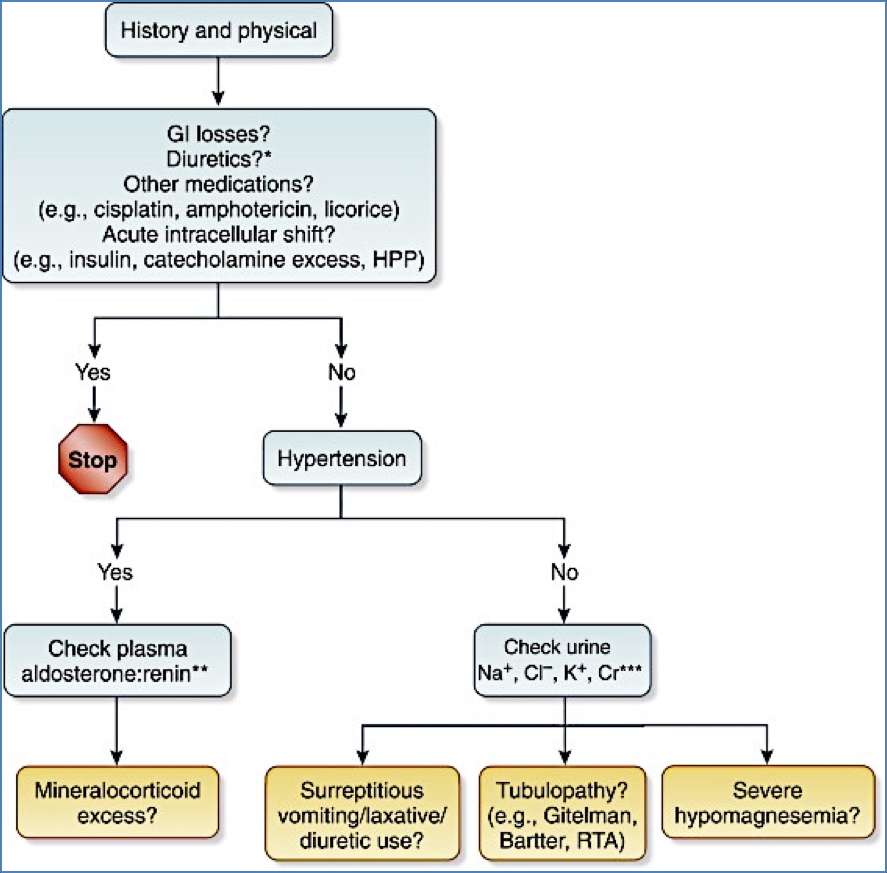
Hypokalaemia
- Definition: Low serum potassium
- Causes:
- Poor intake
- Excess losses (e.g. vomiting, diarrhoea, diuretics)
- Effects:
- Rapid repolarisation → decreased nerve/muscle excitability
- Cardiac irritability → dysrhythmias
- Treatment:
- Correct underlying cause
- Potassium supplements
Calcium (Ca²⁺)
Note: Calcium is vital for cardiac, neuromuscular, and skeletal function.
Hypercalcaemia
- Definition: Elevated serum calcium
- Causes:
- Increased intake
- Decreased excretion
- Bone resorption
- Effects:
- Shortened cardiac AP plateau → arrhythmias
- Muscle weakness
- Treatment:
- IV fluids + salt loading
- Followed by loop diuretics to enhance calcium excretion
Hypocalcaemia
- Definition: Low serum calcium
- Causes:
- Inadequate intake
- Renal loss
- Effects:
- Prolonged cardiac depolarisation
- Muscle twitching, cramps
- Treatment:
- IV calcium replacement
Phosphates (HPO₄²⁻)
Note: Phosphates are key for ATP synthesis and bone mineralisation.
Hyperphosphataemia
- Definition: Elevated phosphate levels
- Causes:
- Hypoparathyroidism (↓ PTH)
- Renal failure (retention of phosphate)
- Effects:
- Precipitation of calcium salts → hypocalcaemia, tissue calcification
- Treatment:
- Phosphate binders
- Dietary restriction
Hypophosphataemia
- Definition: Low phosphate levels
- Causes:
- Poor intake
- Chronic alcoholism
- Long-term antacid use
- Effects:
- ↓ ATP production → muscle weakness, cardiac and neurological dysfunction
- Treatment:
- IV phosphate replacement
Plasma Proteins
Hyperproteinaemia
- Rare and typically asymptomatic
Hypoproteinaemia
- Causes:
- Liver failure
- Protein malnutrition
- Burns
- Proteinuria in kidney failure
- Effects:
- ↓ Plasma oncotic pressure → generalised oedema

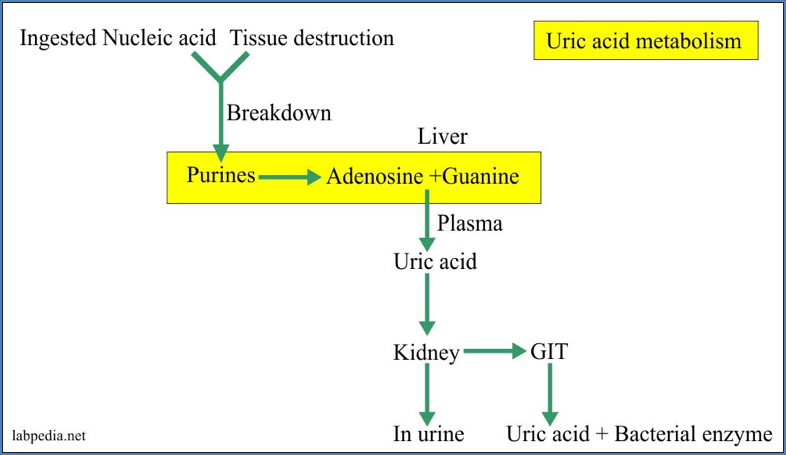
Uric Acid
Hyperuricaemia
- Definition: Elevated blood uric acid
- Cause:
- Renal failure → impaired excretion
- Effect:
- Gout – uric acid crystal deposition in joints → inflammatory arthritis
- Treatment:
- Lifestyle modification
- Uric acid-lowering drugs (not detailed in original notes)
Summary – Electrolyte Imbalances
Electrolyte imbalances such as hypernatraemia, hypokalaemia, or hyperphosphataemia can have profound physiological consequences, including arrhythmias, seizures, muscle weakness, and oedema. Effective management depends on identifying the underlying cause, correcting fluid status, and replacing or restricting the relevant ion. For a broader context, see our Renal Overview page.