Table of Contents
Overview – Renal Physiology
Renal physiology encompasses the complex and vital processes by which the kidneys regulate fluid balance, electrolytes, blood pressure, and acid-base homeostasis. The kidneys also play critical roles in erythropoiesis and vitamin D activation. An understanding of renal physiology is fundamental to interpreting renal function tests, understanding disease mechanisms, and managing common clinical conditions such as hypertension and acidosis.
Physiological Functions of the Kidney
- Fluid conservation
- Electrolyte balance (Na⁺, K⁺, PO₄³⁻, HCO₃⁻)
- Excretion of metabolic waste (urea, creatinine, bilirubin)
- Acid-base homeostasis (H⁺/HCO₃⁻ balance)
- Blood pressure regulation (via fluid volume & renin-angiotensin system)
- Erythropoiesis (via erythropoietin secretion)
- Vitamin D activation
Hormonal Regulation in Renal Physiology
- Renin
- Secreted by juxtaglomerular cells in response to renal hypoperfusion
- Stimulates conversion of angiotensinogen to angiotensin I
- Also causes afferent arteriole vasodilation to improve kidney perfusion
- Angiotensin II
- Produced in the lungs from angiotensin I
- Causes systemic vasoconstriction → ↑BP
- Constricts efferent arterioles → maintains GFR
- Stimulates aldosterone secretion
- Aldosterone
- Secreted by adrenal cortex in response to angiotensin II, hyperkalaemia, or hyponatraemia
- Promotes Na⁺ reabsorption, K⁺ excretion, and water reabsorption
- Anti-Diuretic Hormone (ADH)
- Released from posterior pituitary in response to increased plasma osmolality
- Increases water reabsorption in the collecting ducts → ↑plasma volume, ↓urine output
Urine Production and Excretion
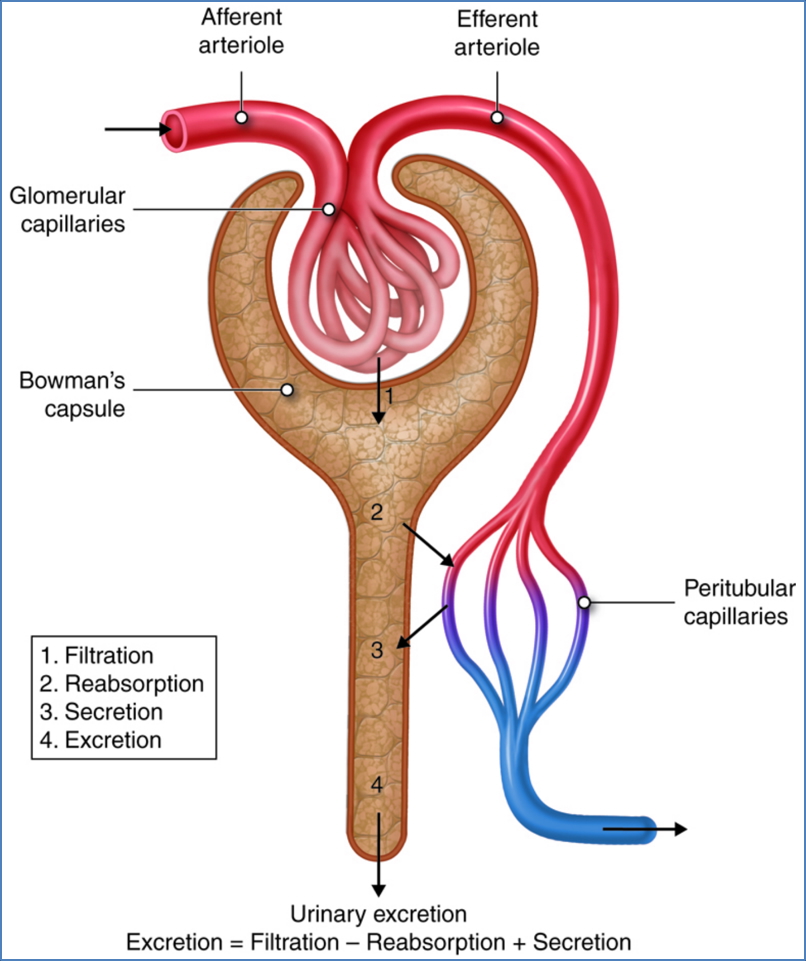
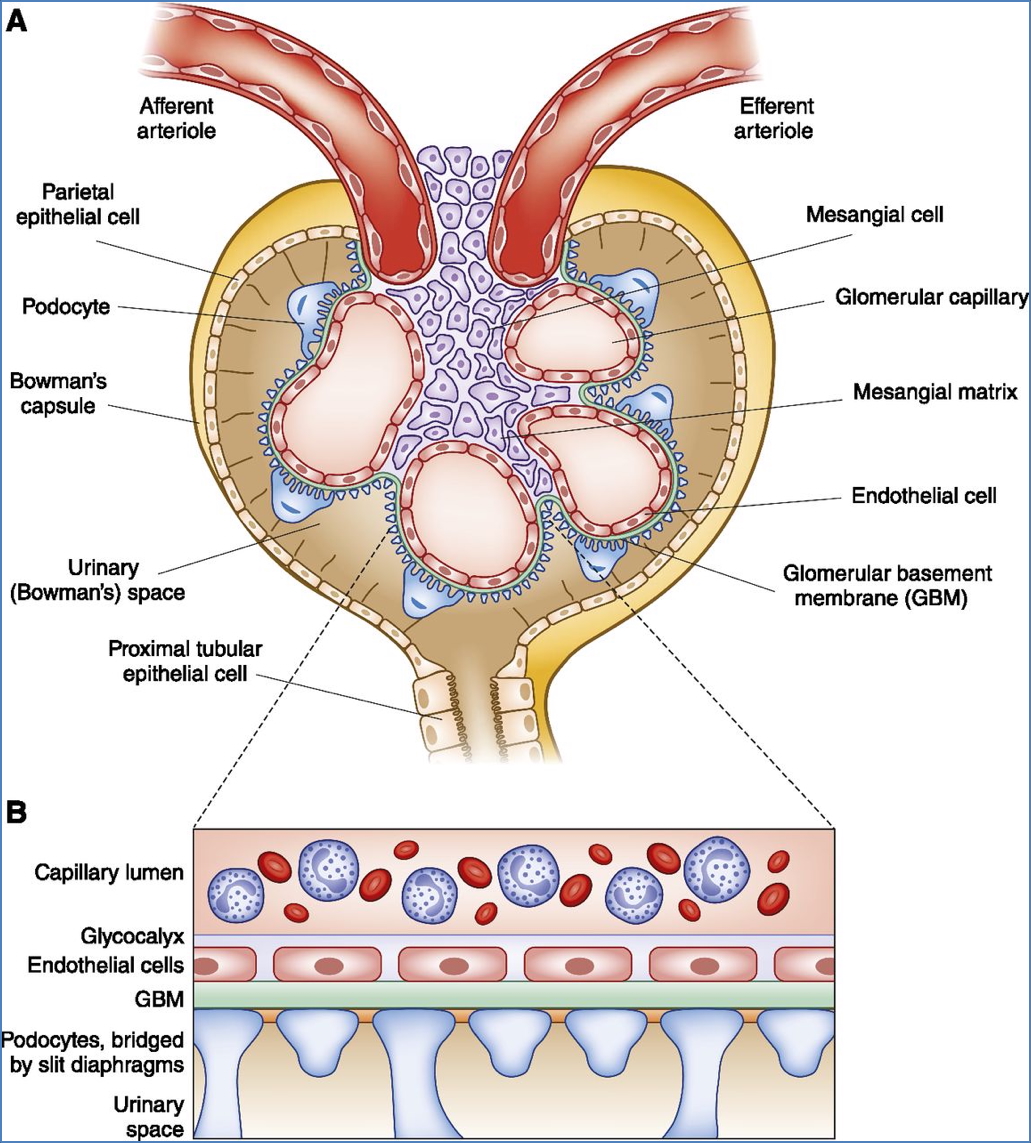
Step 1 – Glomerular Filtration
- Passive, non-selective filtration of blood plasma into Bowman’s capsule
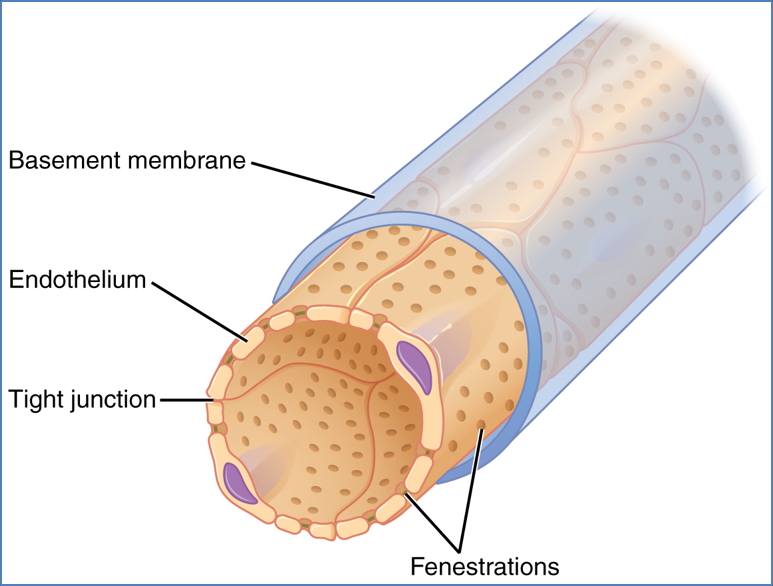
- Occurs across 3 layers:
- Capillary endothelium
- Glomerular basement membrane
- Podocytes (visceral layer of capsule)

2. OpenStax College, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons
3. Front. Physiol., 02 June 2021 | https://doi.org/10.3389/fphys.2021.689083
- Filtrate resembles plasma, but is protein-free (if membrane intact)
- Filtration rate (GFR):
- Depends on net hydrostatic pressure and colloid osmotic pressure
- Also influenced by membrane permeability and filtration surface area
- Kidneys filter ~180L/day from ~1L/min blood flow (≈25% of cardiac output)
- Most of this filtrate is reabsorbed

- GFR Regulation:
- ↓GFR via sympathetic NS, endothelin, adrenaline
- ↑GFR via prostaglandins, nitric oxide, bradykinin
- Angiotensin II maintains GFR by efferent arteriole constriction
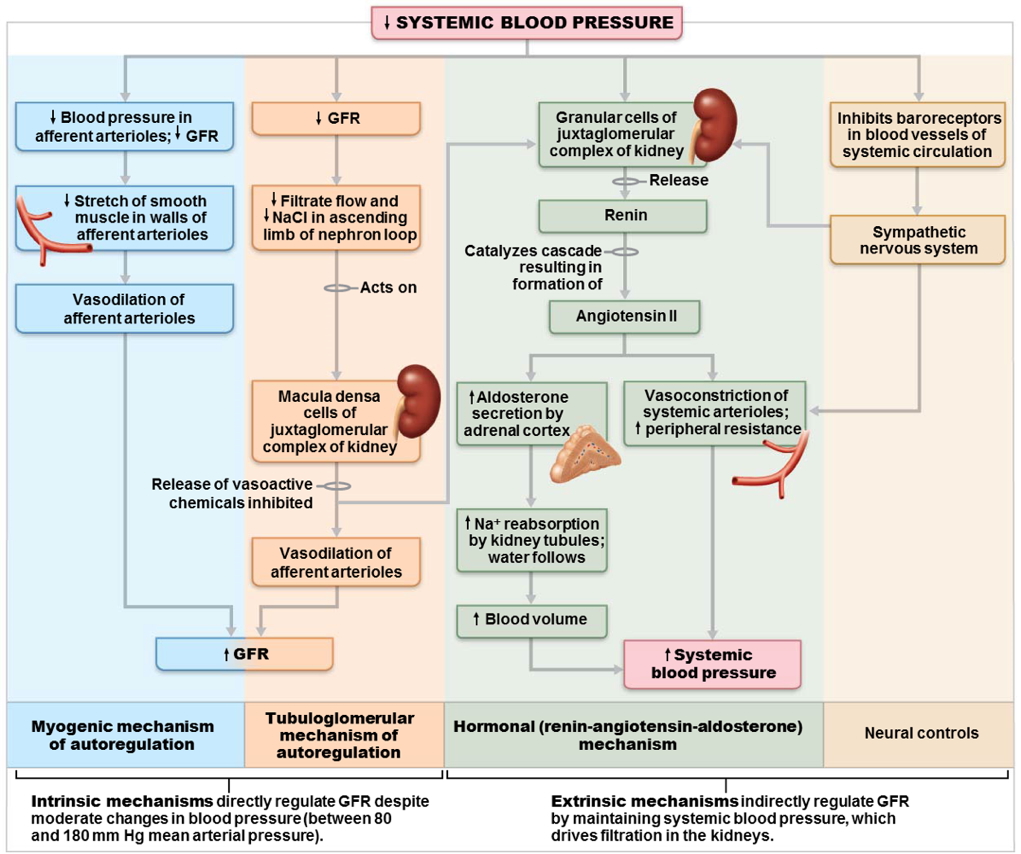
- Autoregulation:
- Myogenic: smooth muscle contracts when stretched
- Metabolic: low oxygen or nutrients → vasodilation
- Maintains stable GFR across varying arterial pressures

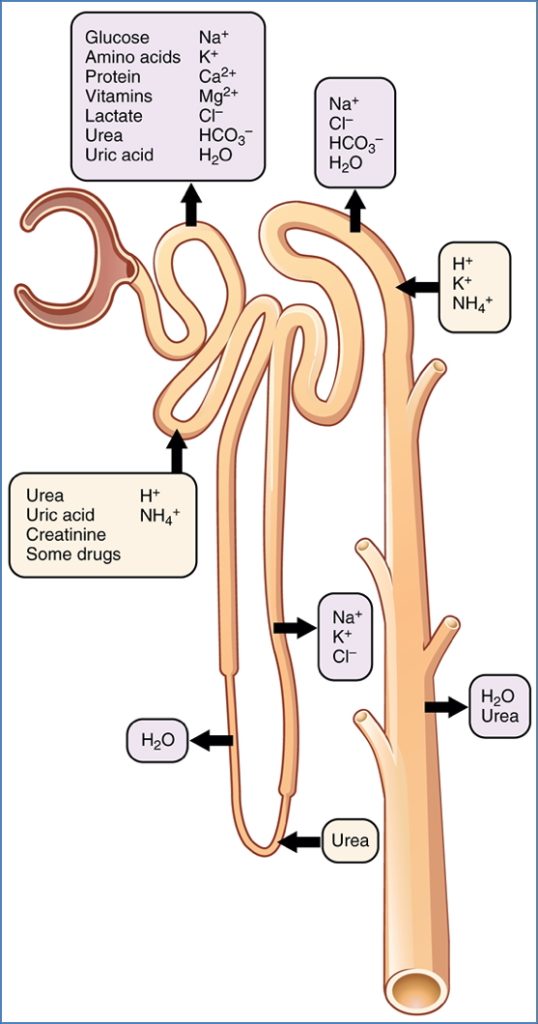
Step 2 – Tubular Reabsorption
- Selective reabsorption of substances into peritubular capillaries
- ~99% of filtrate is reabsorbed
- Routes:
- Transcellular (through cells)
- Paracellular (between cells)
- Passive processes (e.g. osmosis for water)
- Active transport:
- Eg: Na⁺ via Na⁺/K⁺-ATPase
- All transporters have maximum capacities (e.g. glucose spills into urine in diabetes)
- Example: Na⁺ reabsorption in ascending limb
- Stepwise: Passive diffusion into tubule cell → Active transport to interstitium → Uptake by capillaries

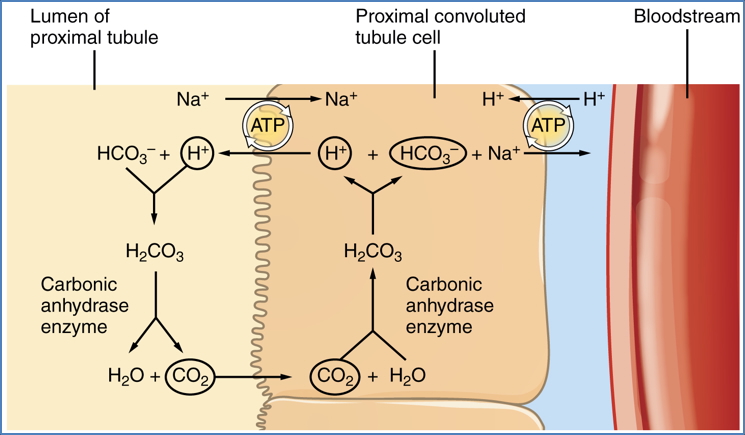
2. Reabsorption of Bicarbonate from the PCT
(OpenStax College, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons)
Step 3 – Tubular Secretion
- Active transfer of substances from capillaries → tubules
- Important for:
- Eliminating drugs (e.g. penicillin)
- Removing poorly filtered substances
- K⁺ and H⁺ secretion (acid-base regulation)
- Sites of secretion:
- Proximal tubule: organic acids/bases
- Distal tubule & collecting duct: K⁺, H⁺, toxins
Micturition Reflex (Urination)
- Reflex pathway: spinal-cord based
- Voluntary control develops by 2–3 years (via cortical inhibition)
- Reflex initiation:
- Bladder fills → stretch receptors fire → brain interprets urge
- Conscious relaxation of external sphincter → detrusor contracts → urine released
- Phases:
- Storage phase: bladder relaxed, sphincters contracted
- Voiding phase: bladder contracts, sphincters relax
- Clinical relevance:
- Neurological damage → incontinence
- Infants rely on involuntary pathway
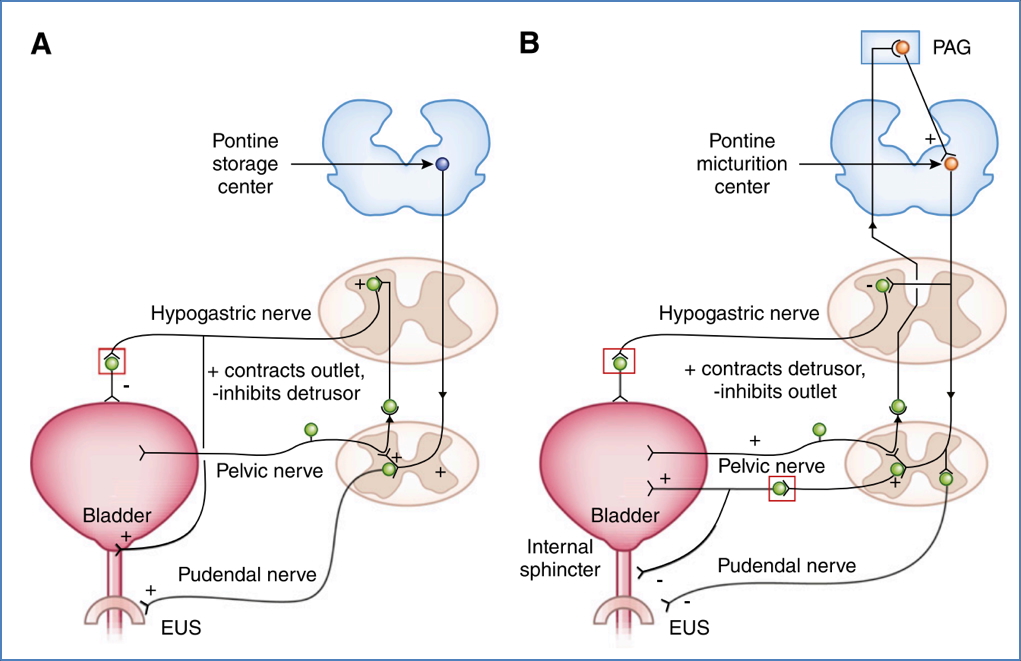

2. OpenStax College, CC BY 3.0 <https://creativecommons.org/licenses/by/3.0>, via Wikimedia Commons
Summary – Renal Physiology
Renal physiology includes the filtration of blood, reabsorption and secretion of solutes, and tightly regulated hormonal control of fluid and electrolyte homeostasis. The kidneys maintain acid-base balance, regulate blood pressure, and contribute to haematopoiesis and vitamin D activation. A clear understanding of renal physiology is critical to managing electrolyte disturbances and renal pathology. For a broader context, see our Renal Overview page.