Table of Contents
Overview – Renal Pathology
An overview of renal pathology encompasses a wide spectrum of diseases that affect the glomeruli, tubules, interstitium, and renal vasculature. While certain pathologies predominantly affect specific components—such as immunologically mediated glomerular damage or toxin-induced tubular injury—these processes often converge, resulting in chronic kidney damage and ultimately renal failure. Understanding these overlapping mechanisms is essential for diagnosing and managing kidney disease.
Renal Structures Affected by Disease
- Glomeruli – commonly affected by immune-mediated injury
- Tubules & Interstitium – typically injured by toxins or infections
- Blood Vessels – often secondarily affected by damage in other compartments
- Interdependence – damage to one area usually leads to downstream dysfunction in others → progression to chronic renal failure
Functional Reserve of the Kidneys
- Only one kidney is needed to sustain life
- Each kidney has more capacity than physiologically required
- Significant damage must occur before clinical symptoms appear
- Once lost, renal function is largely irreversible
Stages of Chronic Renal Failure
1. Diminished Renal Reserve
- GFR ≈ 50% of normal
- BUN and creatinine = normal
- Asymptomatic; reduced reserve but no overt dysfunction
2. Renal Insufficiency
- GFR = 20–50%
- Elevated BUN and creatinine (“azotaemia”)
- Anaemia (↓ erythropoietin)
- Polyuria (↓ H₂O retention)
- Hypertension (fluid overload + renin-mediated vasoconstriction)
3. Renal Failure
- GFR < 20%
- Markedly elevated BUN and creatinine → “uraemia”
- Uraemia = toxic to CNS
- Anaemia, polyuria, hypovolaemia
- Electrolyte disturbances:
- Hyperkalaemia
- Hyperphosphataemia
- Hypocalcaemia
- Secondary effects:
- Osteoporosis
- Haematuria
4. End-Stage Renal Disease (ESRD)
- GFR < 5%
- Terminal uraemia; requires dialysis or transplant
Major Risk Factors
Hypertension
- ↑ glomerular pressure → capillary wall damage
- → Glomerulosclerosis
- → Tubular necrosis → inflammation → progressive failure
Diabetes Mellitus
- Hyperglycaemia → glycosylated proteins damage capillaries
- → Microvascular inflammation → tubular necrosis
- → Inflammatory cascade → chronic kidney disease
Clinical Complications of Renal Disease
Electrolyte Imbalances
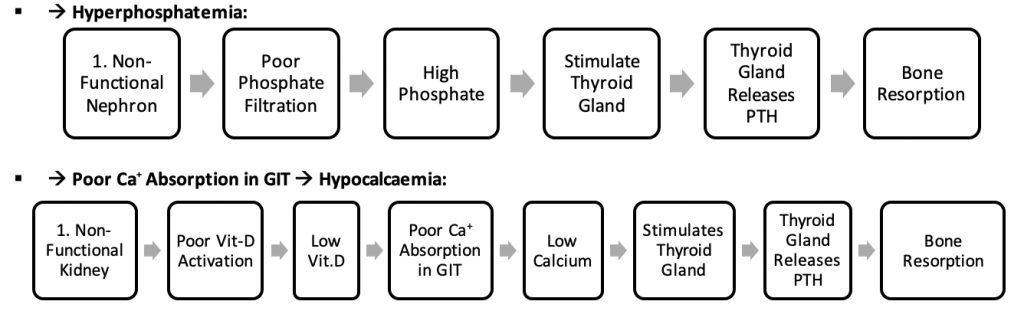
- Hyperphosphataemia:
- ↓ excretion → phosphate retention
- CaPO₄ tissue deposition → calcification
- Stimulates PTH → bone resorption
- Hyperkalaemia:
- ↓ excretion → high serum K⁺
- Risk of fatal arrhythmias
- Hypocalcaemia:
- ↓ Vit D activation by kidney → ↓ gut Ca²⁺ absorption
- PTH-mediated bone resorption
- Risk of urinary calculi, arrhythmias
Renal Bone Disease
- ↓ phosphate clearance + ↓ Vit D →
- ↑ phosphate → hypocalcaemia → bone demineralisation
- Stimulates PTH → worsening bone loss
Haematological
- Anaemia:
- ↓ erythropoietin → ↓ RBC production
Fluid Balance
- Dehydration:
- Tubular dysfunction → poor urine concentration → water loss
Uraemia
- Elevated urea/creatinine → systemic toxicity:
- CNS: confusion, drowsiness, seizures
- GI: nausea, vomiting
- Serous membranes: uraemic pericarditis
- Skin: pruritus (urea excretion via sweat)
Summary – Renal Pathology Overview
An overview of renal pathology involves glomerular, tubular, interstitial, and vascular injury, often interrelated and progressing toward chronic renal failure. The kidneys’ strong functional reserve means symptoms only appear late, but once damaged, the decline is typically irreversible. Understanding staging, risk factors like hypertension and diabetes, and common systemic complications is key to managing kidney disease. For a broader context, see our Renal Overview page.