Table of Contents
Overview – Cervical Cancers
Cervical cancers, including CIN1 (LSIL) and CIN2–3 (HSIL), are almost universally caused by persistent infection with high-risk human papillomavirus (HPV), particularly types 16, 18, and 45. These lesions represent a spectrum from mild dysplasia (LSIL) to severe pre-cancerous changes (HSIL), with potential to progress to invasive carcinoma. Early detection through Pap screening and HPV vaccination dramatically reduces the risk of progression and mortality.
Definition
Cervical intraepithelial neoplasia (CIN) refers to dysplastic changes in the squamous epithelium of the cervix, classified as:
- CIN1 / LSIL (Low-grade Squamous Intraepithelial Lesion)
- CIN2–3 / HSIL (High-grade Squamous Intraepithelial Lesion)
Aetiology
- Human Papillomavirus (HPV) infection – especially types 16, 18, 45, 31, and 33
- Direct contact/sexual transmission
- Other risk factors:
- Promiscuity
- Family history
- Increased estrogen exposure (early menarche, late menopause, nulliparity, obesity, HRT)
- Smoking
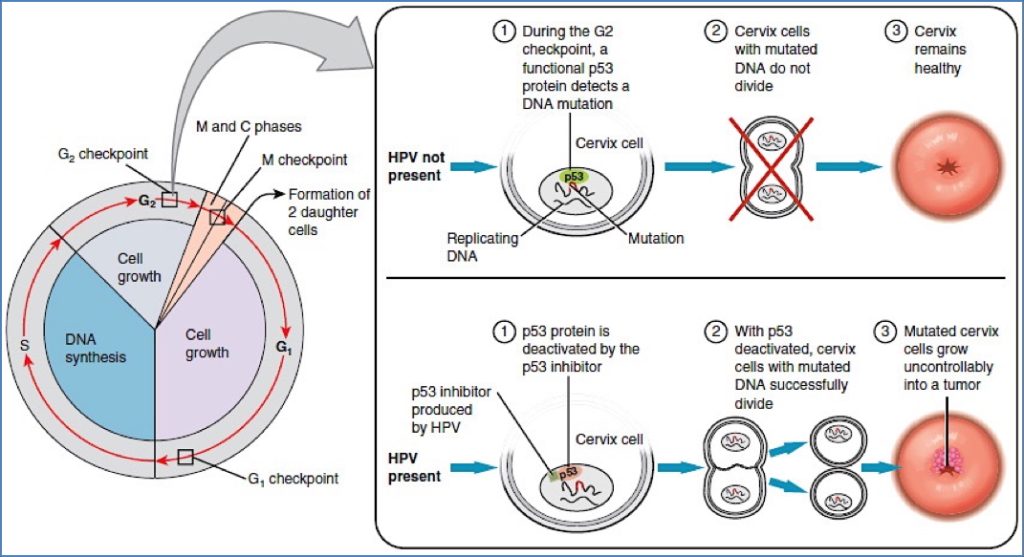
Pathogenesis
- HPV infection introduces viral proteins:
- E6 inhibits p53 (tumour suppressor gene)
- E7 inhibits RB (tumour suppressor gene)
- → Cell-cycle dysregulation → Dysplasia → Invasive carcinoma
- Estrogens act as a proliferation promoter, enhancing transformation risk
Morphology
LSIL (CIN1)
- Macro: Small, well-defined flat leucoplakia
- Micro:
- Koilocytosis – perinuclear halo, wrinkled nucleus, viral inclusions
- Mild nuclear enlargement
- Atypia limited to basal third of the epithelium
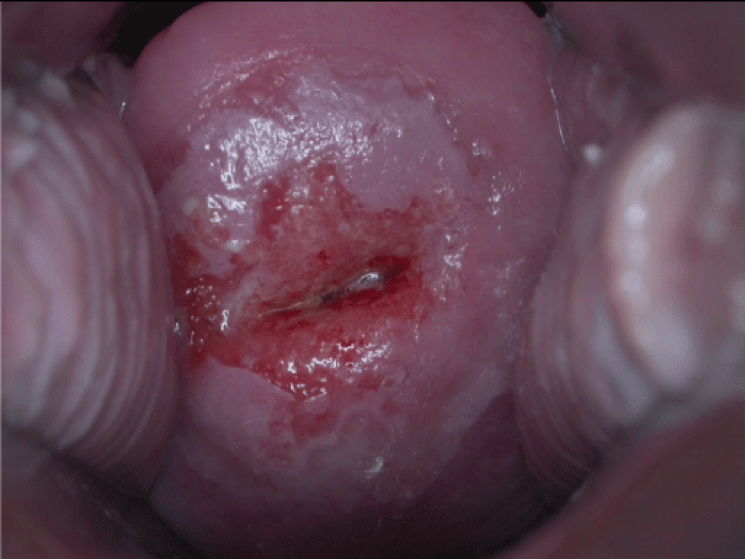
HSIL (CIN2–3)
- Macro:
- CIN2: Larger, clearly-defined flat leucoplakia
- CIN3: Patchy, poorly defined areas with haemorrhage
- Micro:
- Koilocytosis
- Full-thickness replacement with dysplastic squamous cells (CIN3)

Clinical Features
- Common in women aged 40–50 years
- Usually asymptomatic
- Advanced disease may present with:
- Post-coital bleeding
- Vaginal discharge
Investigations
- Pap smear (screening only)
- Colposcopy + directed biopsy – diagnostic gold standard
- Staging (via CT/MRI):
- Stage I: Confined to cervix
- Stage II: Extension beyond cervix
- Stage III: Pelvic or vaginal involvement
- Stage IV: Distant spread (e.g. liver, lungs, bone)
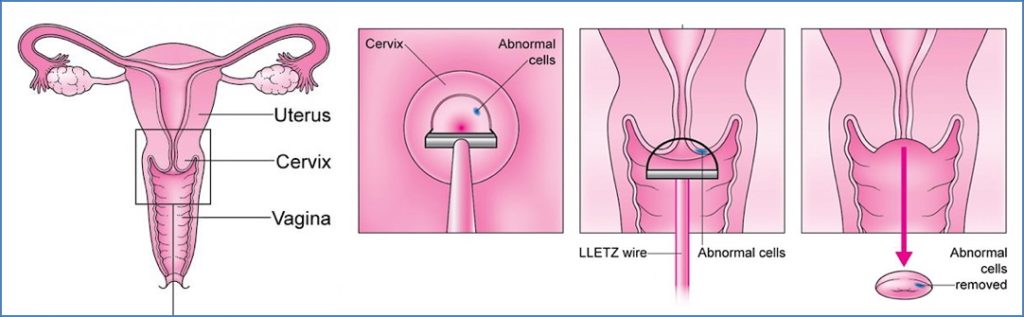
Management
- CIN1 (LSIL): Watchful waiting and follow-up
- CIN2–3 (HSIL):
- Excision of transformation zone via:
- LLETZ/LEEP (Large Loop Excision)
- Cold knife cone biopsy
- Excision of transformation zone via:
- Invasive Cancer:
- Total hysterectomy ± oophorectomy + pelvic lymph node dissection
- ± Radiotherapy (EBRT or brachytherapy)
- ± Chemotherapy for advanced disease
Prognosis
- CIN1: >95% regress spontaneously
- CIN3: ~70% progress to invasive cancer without treatment
- 5-year survival:
- Stage I: >80%
- Stage IV: ~10%
Prevention
Primary Prevention
- HPV vaccination (Gardasil) – covers HPV 6, 11, 16, and 18
- Recommended for girls aged 9–13 years
- Schedule: 3 IM doses at 0, 2, and 6 months
- Vaccination does not eliminate need for screening
Secondary Prevention
- Pap smear screening
- Every 2 years from age 18 or onset of sexual activity
- Ideal timing: 1st week after menstruation
- Abnormal results → Colposcopy and biopsy
- Follow-up:
- Normal → repeat in 2 years
- LSIL with normal recent smear → repeat in 12 months
- LSIL with no recent smear or HSIL → immediate colposcopy

Colposcopy Indicators
- Abnormal Pap result (LSIL/HSIL)
- Assessment of the transformation zone using:
- Acetic acid – dysplastic cells turn white
- Lugol’s iodine – dysplastic areas remain unstained
- Punch biopsy – confirms CIN grade

Summary – Cervical Cancers
Cervical cancers, including CIN1 and CIN2–3, result from HPV-mediated disruption of tumour suppressor pathways, progressing from low-grade lesions to high-grade dysplasia and potentially invasive carcinoma. Prevention via HPV vaccination and regular Pap screening is highly effective. For further detail, see our Reproductive Health Overview page.