Table of Contents
Overview – Female Reproductive Anatomy
Understanding the female reproductive anatomy is essential for clinical assessment, gynaecological examination, and understanding pathologies such as cervical cancer, ectopic pregnancy, or pelvic organ prolapse. This page provides a clear and high-yield review of the internal and external reproductive structures, blood supply, pelvic floor, cervical histology, and the breast — all crucial for OSCE stations and clinical rotations.
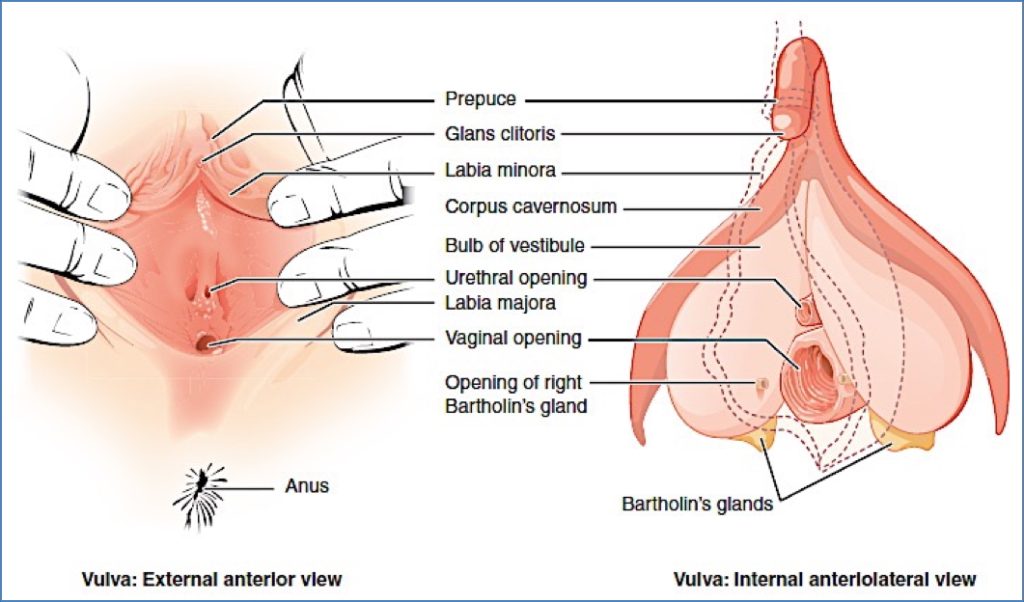
External Genitalia (Vulva)
- Labia majora & labia minora: External folds of skin protecting the vestibule.
- Clitoris: Erectile organ formed from paired corpora cavernosa; covered by the prepuce.
- Urethral orifice: External opening of the urethra.
- Vaginal opening: Posterior to the urethral meatus.
- Bartholin’s glands: Located near vaginal opening; secrete mucus for lubrication.
Internal Genitalia
Vagina
- Muscular tube extending from the vulva to the cervix.
- Functions in intercourse, menstruation, and childbirth.
Uterus
- Divided into:
- Fundus: Dome-shaped superior portion.
- Body: Central portion.
- Cervix: Lower, narrow part with:
- External os, cervical canal, and internal os.
- Uterine wall layers:
- Perimetrium: Outer serous layer.
- Myometrium: Thick muscular layer.
- Endometrium: Inner mucosal layer responsive to hormones.
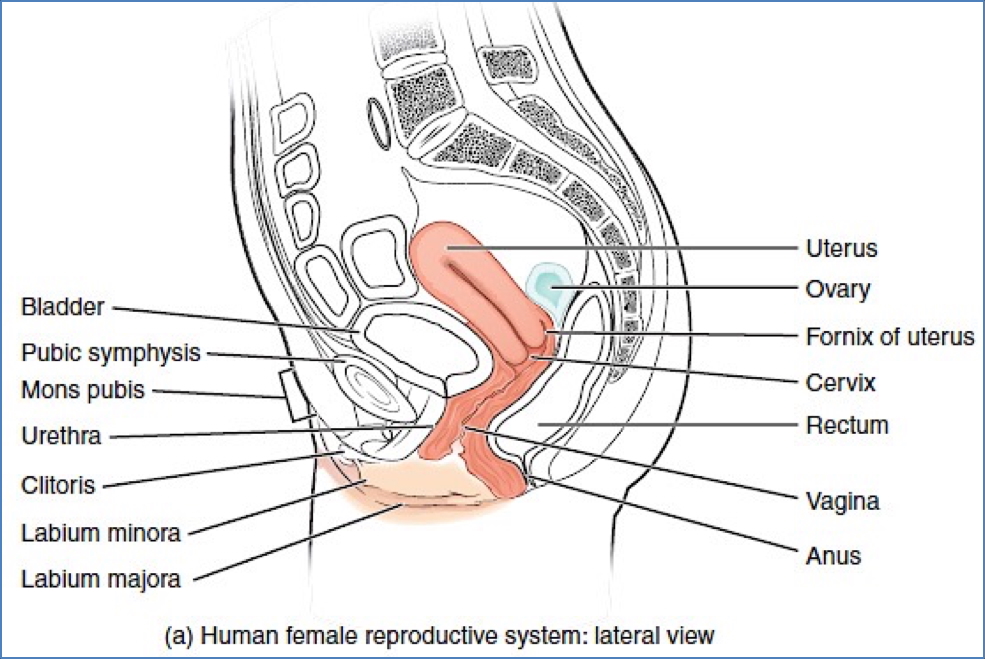
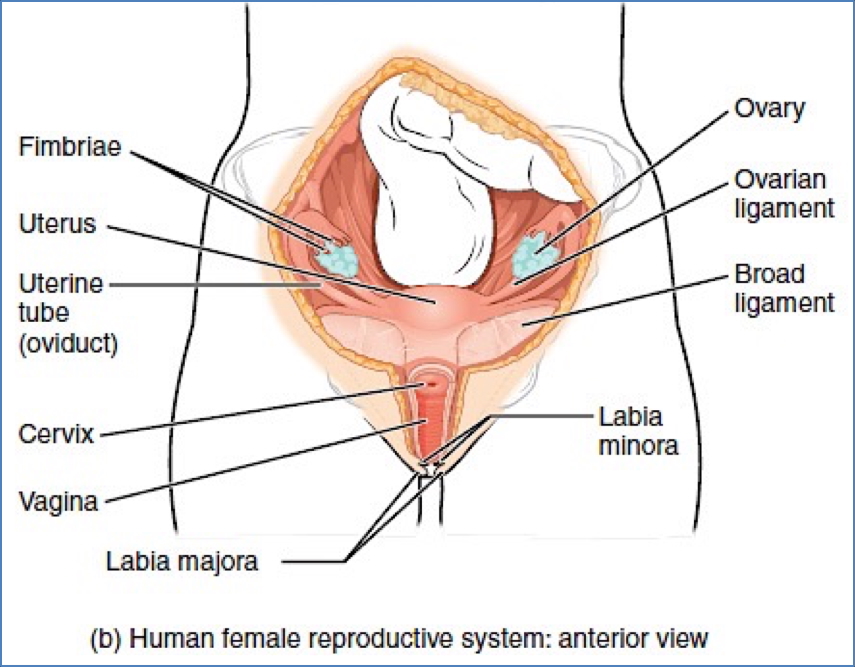
Fallopian (Uterine) Tubes
- Site of fertilisation.
- Divided into:
- Infundibulum with fimbriae → captures ovulated oocyte.
- Ampulla, isthmus, and intramural segments.
Ovaries
- Female gonads; produce oocytes and secrete oestrogen and progesterone.
- Anchored by ligaments and supported by surrounding musculature.

Blood Supply to Reproductive Organs
- Internal iliac artery (branch of common iliac):
- Supplies:
- Uterine artery
- Vaginal artery
- External genitalia
- Supplies:
- Ovarian artery (branch of abdominal aorta):
- Supplies:
- Ovaries
- Fallopian tubes
- Uterus (partially)
- Supplies:
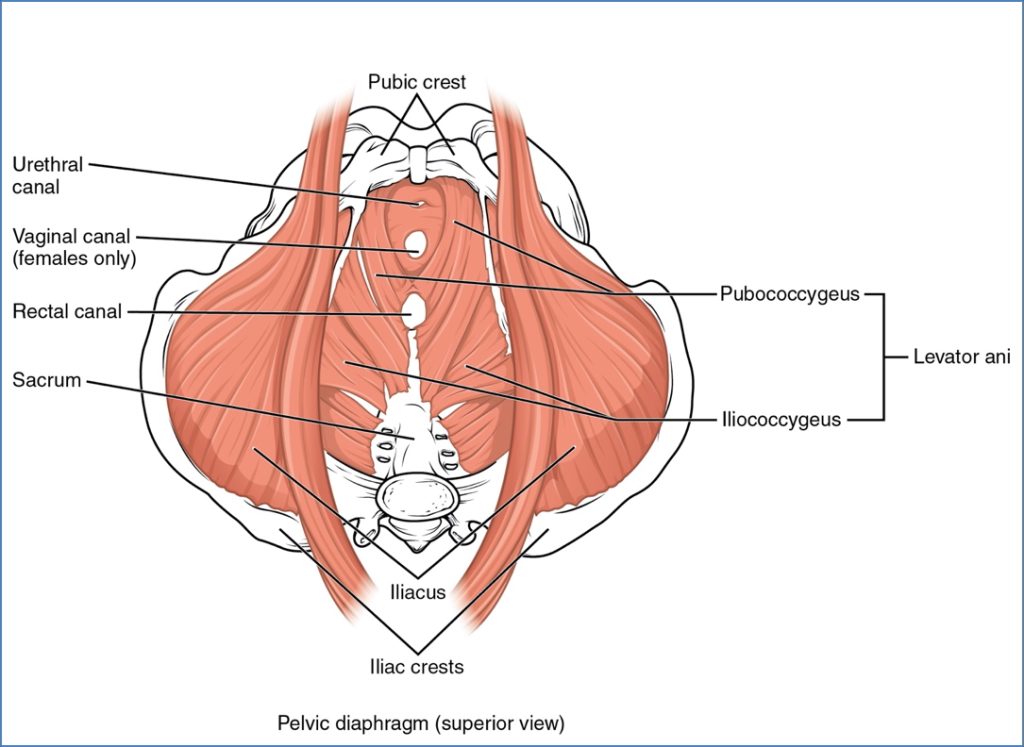
Pelvic Floor Anatomy
- Pelvic diaphragm supports pelvic organs and maintains continence.
- Major muscles:
- Levator ani (anterior):
- Pubococcygeus
- Iliococcygeus
- Coccygeus (ischiococcygeus) – posterior
- Piriformis – posterior-lateral pelvic wall
- Levator ani (anterior):
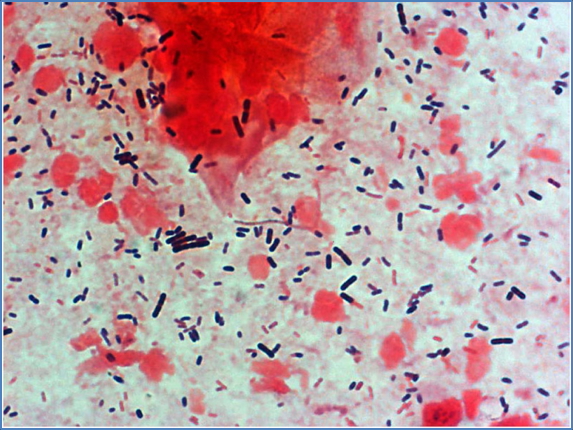
Vaginal Flora
Female Vaginal Flora
- Dominated by Lactobacillus spp. (gram-positive rods).
- Produce lactic acid, maintaining acidic pH.
- Protects against bacterial vaginosis and yeast infections.
Male Urethral Flora (for comparison)
- Sparse; includes Staphylococcus epidermidis, Streptococci, Ureaplasma urealyticum.
Cervical Anatomy & Histology
- Transformation Zone (TZ):
- Site where columnar epithelium of endocervix transitions to squamous epithelium of ectocervix.
- Most common site for cervical cancer.
- During puberty: Columnar cells migrate outward and undergo squamous metaplasia due to acidic vaginal environment.
- Normal Histology:
- Endocervix: Simple columnar epithelium.
- Ectocervix: Stratified squamous epithelium.

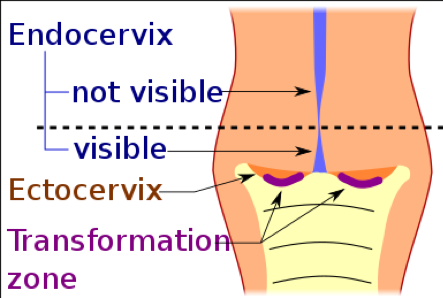
2. Mikael Häggström, M.D. – Author info – Reusing images- Conflicts of interest: NoneMikael Häggström, CC0, via Wikimedia Commons
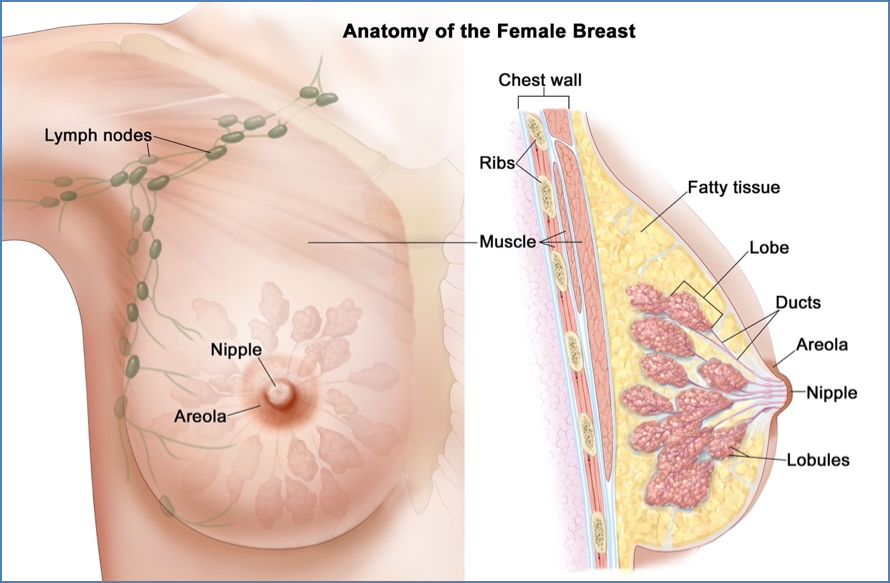
Breast Anatomy
Basic Structure
- Mammary glands exist in both sexes but are only functional in females.
- Located within the superficial fascia, over the pectoralis major.
Components
- Areola: Pigmented skin surrounding the nipple; contains sebaceous glands.
- Nipple: Central projection for milk ejection.
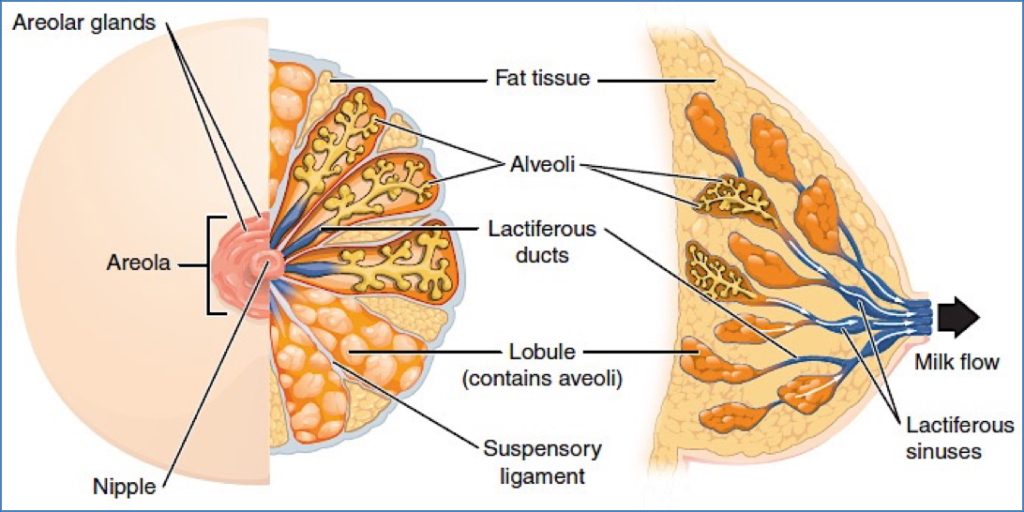
Glandular Organisation
- ~20 lobes → lactiferous ducts → lactiferous sinuses → nipple.
- Each lobe contains lobules with glandular alveoli producing milk during lactation.
Support & Drainage
- Suspensory (Cooper’s) ligaments: Anchor breast to skin and fascia.
- Lymphatic drainage:
- Supraclavicular, infraclavicular, parasternal, pectoral, axillary (primary), central, subscapular.
Summary – Female Reproductive Anatomy
The female reproductive anatomy consists of intricately organised structures including external genitalia, the uterus, ovaries, fallopian tubes, and breast tissue. Each component plays a vital role in reproduction, hormonal regulation, and clinical examination. For a broader context, see our Reproductive Health & Obstetrics Overview pages.