Table of Contents
Overview – Human Immunodeficiency Virus
Human Immunodeficiency Virus (HIV) is a retrovirus that primarily targets CD4+ T-lymphocytes, resulting in progressive immune suppression and a heightened vulnerability to opportunistic infections and certain cancers. HIV is transmitted through blood, body fluids, and from mother to child. Without treatment, it leads to Acquired Immunodeficiency Syndrome (AIDS), the advanced stage of HIV infection. The virus is known for its rapid mutation rate, long asymptomatic phase, and complex interaction with the host immune system, making early detection and lifelong treatment essential.
Definition
HIV is a blood-borne retroviral infection that causes chronic, progressive immune system dysfunction by destroying CD4+ T-helper cells. If untreated, HIV progresses to AIDS, defined by severe immunosuppression and opportunistic infections.
Aetiology
- Caused by the Human Immunodeficiency Virus (HIV)
- Two major types:
- HIV-1 – more virulent and globally widespread
- HIV-2 – less virulent, mostly found in West Africa

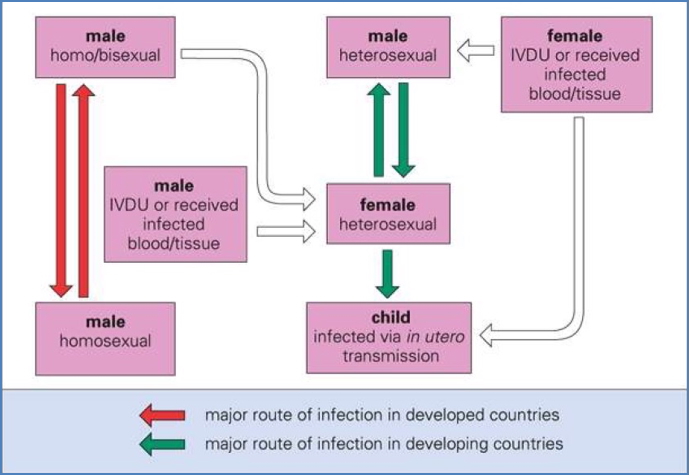
Transmission
- Blood – e.g. intravenous drug use (IVDU), transfusions
- Body fluids – semen, vaginal secretions (especially via anal sex due to mucosal fragility)
- Vertical – transplacental, peripartum, and via breastmilk
- Transmission risks are influenced by:
- Viral load (titre)
- Mucosal damage or inflammation (e.g. concurrent STIs)
- Type of sexual contact (highest in anal > vaginal > oral)
Pathogenesis
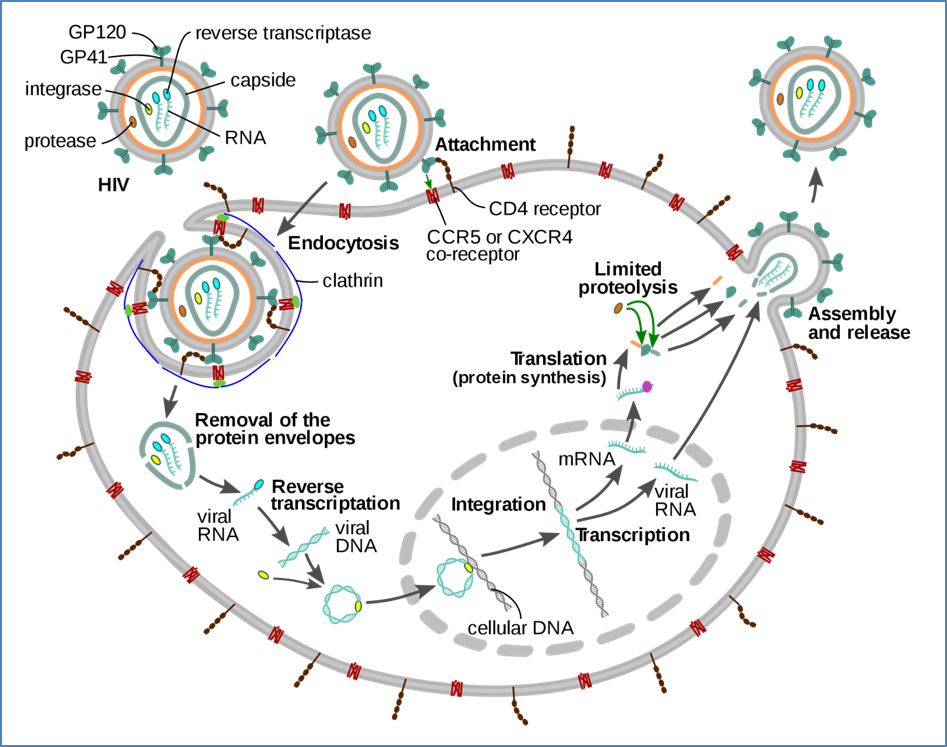
- HIV is lymphotropic, targeting CD4+ T-cells using the gp120 envelope glycoprotein and co-receptors:
- CCR5 – macrophage-tropic strains
- CXCR4 – T-cell-tropic strains
- Viral replication steps:
- Viral binding to CD4
- Fusion and internalisation
- Reverse transcription of ssRNA → dsDNA via reverse transcriptase
- Integration into host genome
- Transcription, translation, assembly, and viral budding
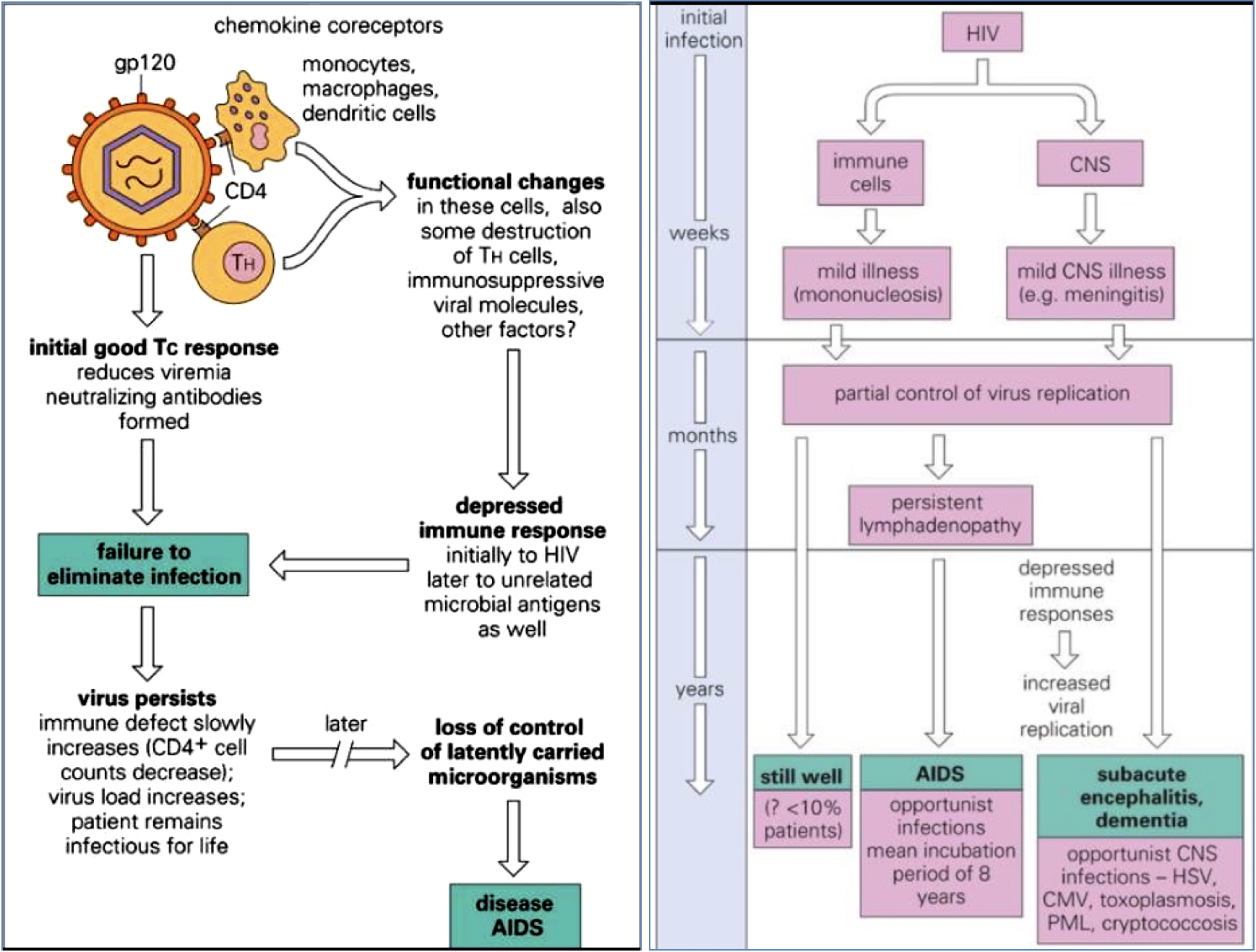
- The immune system is progressively weakened through:
- CD4+ T-cell lysis
- Syncytia formation
- Apoptosis
- Immune-mediated killing of infected T-cells
- Leads to ↓IFNγ, ↓macrophage activation, ↓antibody production, ↓CD8+ T-cell activity
2. Unattributable
Clinical Features
Natural History (Without Treatment):
- Acute Infection (1–2 months post-exposure)
- Flu-like illness, maculopapular rash, high viremia
- Antibodies detectable after ~2.5 months
- Chronic Asymptomatic Phase (2–4 years)
- Clinical latency, gradual CD4+ decline
- Viral set point established
- Symptomatic Chronic Infection (≈ 8 years)
- HIV quasispecies outnumber immune capacity
- Minor opportunistic infections, fatigue
- AIDS (≈ 10–12 years)
- CD4 count <200 cells/mm³
- Severe immunosuppression
- Opportunistic infections, AIDS dementia, cancers (e.g. Kaposi’s sarcoma)

Investigations
- Serology – HIV Ab/Ag Combo tests
- PCR – Quantitative HIV RNA (viral load)
- CD4 count – Marker of disease progression
- Resistance testing – Guides ART choices
Morphology
- HIV virion:
- Icosahedral capsid
- Envelope with glycoproteins (gp120, gp41)
- 2 ssRNA strands
- Reverse transcriptase, integrase, and protease enzymes
- Key genes: gag, pol, env
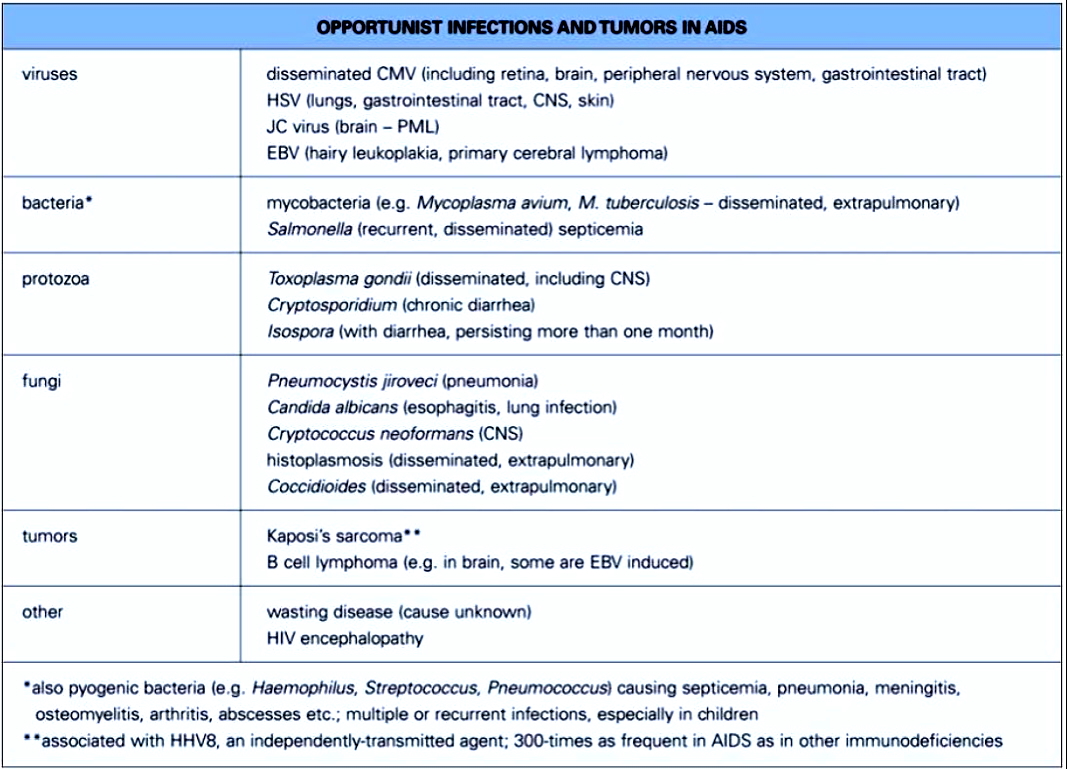
Complications
- Infectious – e.g. TB, CMV, Candida, Pneumocystis pneumonia
- Neoplastic – e.g. Kaposi’s sarcoma, lymphoma
- Neurological – e.g. HIV encephalopathy, AIDS dementia
- Renal & cardiac involvement

Management
Antiretroviral Therapy (ART):
- Combination therapy is standard (typically 3+ drugs):
- Fusion inhibitors – e.g. Maraviroc (CCR5 antagonist)
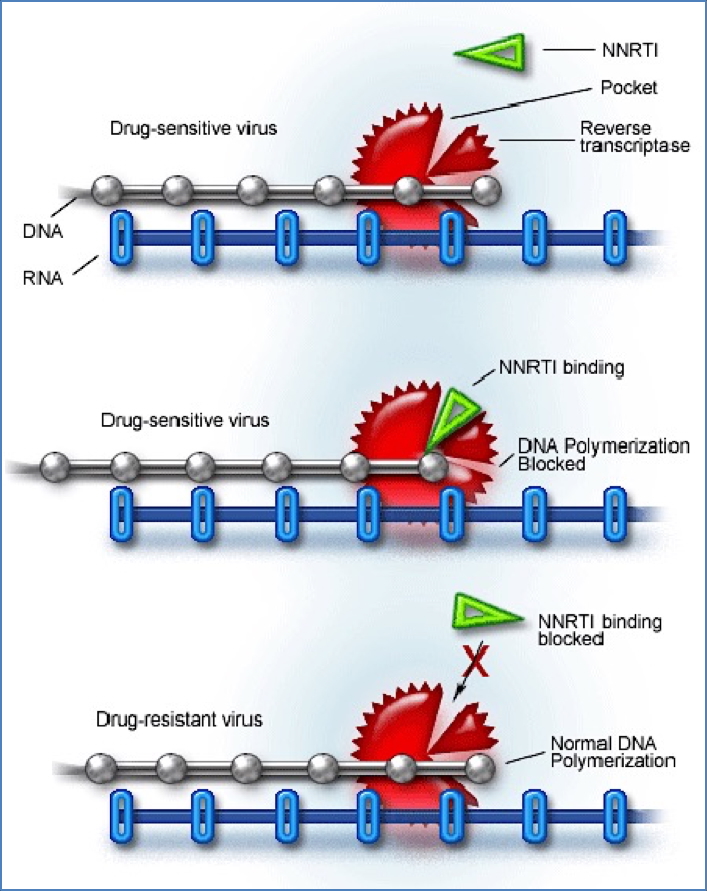
- Reverse Transcriptase Inhibitors (RTIs):
- Nucleoside RTIs (NRTIs): zidovudine, lamivudine
- Non-nucleoside RTIs (NNRTIs): efavirenz, nevirapine
- Protease inhibitors – inhibit viral protein cleavage
- Integrase inhibitors – prevent integration of viral DNA
- ART is lifelong and aims to:
- Suppress viral replication
- Restore/maintain immune function
- Prevent transmission

2. https://clinicalinfo.hiv.gov/en/glossary/protease-inhibitor-pi
Epidemiology
- Sub-Saharan Africa: >66% of global burden
- Developing countries: High heterosexual & vertical transmission
- Developed countries: Male-male transmission, IVDU
- HIV remains a global pandemic, but ART has significantly improved survival and quality of life
Summary – Human Immunodeficiency Virus
Human Immunodeficiency Virus (HIV) causes chronic immune system damage via CD4+ T-cell depletion and leads to AIDS if untreated. Its complex pathogenesis, silent early course, and high mutation rate complicate management. However, with modern antiretroviral therapy, HIV is now a manageable chronic illness. For more on this topic, see our Reproductive Health Overview page.