Table of Contents
Overview – Human Papilloma Virus
Human papilloma virus (HPV) is a common sexually transmitted infection that presents either as genital warts or may lead to the development of cervical and other anogenital cancers. HPV types 6 and 11 are responsible for benign genital warts, whereas types 16, 18, and 45 are high-risk oncogenic strains associated with cervical cancer. Although infection is often asymptomatic, it may have long-term implications. Early detection, vaccination, and patient education are essential components of prevention and management.
Definition
HPV is a DNA virus transmitted through sexual and direct contact, affecting epithelial cells and causing either benign warty lesions or malignancies such as cervical carcinoma.
Aetiology
Low-Risk Types
- HPV 6 & 11 → Genital warts
- Preventable with the Gardasil vaccine
High-Risk Types
- HPV 16, 18 & 45 → Cervical cancer
- Gardasil provides partial protection
Transmission
- Direct contact during vaginal, anal, or oral sex
- Highly contagious
- Can also be spread via fomites (e.g. contaminated surfaces or objects)
Morphology / Pathophysiology
Pathogenesis
- HPV infection via mucosal contact
- 3-month incubation period
- Integration into host genome → cell-cycle dysregulation → epithelial proliferation
Macroscopic Features
- Genital warts (HPV 6/11):
- Papillary or warty lesions on external genitalia, perianal area, or oral mucosa
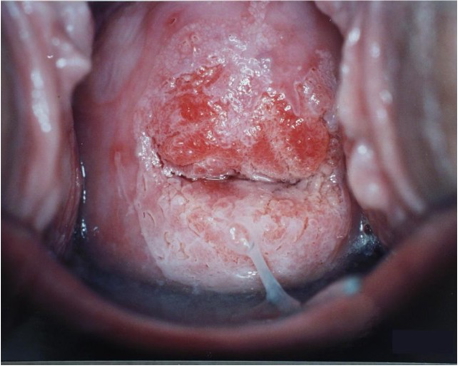
- Cervical cancer (HPV 16/18/45):
- Irregular, ulcerated, or friable cervix
- Loss of smooth contour; visible dysplasia
Microscopic Features
- Warts: Koilocytosis – epithelial cells with perinuclear cytoplasmic clearing (“halo”)
- Cervical cancer:
- Squamous cell carcinoma
- Adenocarcinoma (less common)
Clinical Features
Genital Warts (Types 6/11)
- Often asymptomatic
- Painless papules or exophytic warty lesions
- May coalesce or become irritated

Cervical Cancer (Types 16/18/45)
- Abnormal vaginal bleeding (intermenstrual or post-coital)
- Dyspareunia
- Pelvic pain
- Fatigue and weight loss in advanced disease
- May be asymptomatic in early stages
Investigations
- Pap smear: Screens for cervical epithelial dysplasia
- Cervical biopsy: Histopathological confirmation
- HPV DNA testing: PCR-based detection from cervical swabs
- TamPap: Self-collected HPV DNA sampling
Management
Genital Warts (Types 6/11)
- Topical treatments:
- Podophyllin cream
- Imiquimod (Aldara)
- Procedural options:
- Cryotherapy
- Surgical excision (if extensive or refractory)
- Referral to gynaecology:
- If chronic, recurrent, cervical or rectal involvement
- Counselling:
- Reassurance and education on viral persistence
Cervical Cancer (Types 16/18/45)
- Surgical excision
- +/- Chemotherapy and/or radiotherapy
- Ongoing gynaecologic oncology follow-up
Complications
- Genital warts: Recurrent lesions; persistent subclinical infection
- Cervical cancer: Local invasion, lymphatic and distant metastasis
Prognosis
- Genital warts (Types 6/11):
- Benign
- 70% regress spontaneously within 12 months
- Cervical cancer (Types 16/18/45):
- Malignant and potentially fatal if untreated
Differential Diagnosis
- Pearly penile papules
- Sebaceous hyperplasia
- Vestibular papillomatosis
- Molluscum contagiosum
- Condylomata lata (secondary syphilis)
Summary – Human Papilloma Virus
Human papilloma virus is a prevalent infection with diverse presentations, from benign genital warts to malignant cervical cancer. It is transmitted via direct sexual contact, with certain high-risk strains (HPV 16, 18, 45) linked to oncogenesis. While genital warts are treatable but often recurrent, cervical cancer requires surgical and oncologic management. Early vaccination, screening, and patient education are key to prevention. For a broader context, see our Reproductive Health Overview page.