Table of Contents
Overview – Pelvic Organ Prolapse
Pelvic organ prolapse (POP) refers to the descent of pelvic organs—such as the bladder, uterus, rectum, or small intestine—into or beyond the vaginal canal due to weakened or defective pelvic support structures. It is a common condition, particularly in older, postmenopausal, or multiparous women. Symptoms can significantly impact quality of life, affecting urinary, bowel, and sexual function. Understanding the types, symptoms, and treatment options is key to effective diagnosis and management.
Definition
Pelvic organ prolapse is the protrusion of pelvic organs into or out of the vaginal canal, caused by weakened or defective support structures of the pelvis.
Aetiology
The underlying cause is the incompetence of pelvic support structures, especially the uterosacral ligaments. Contributing factors include:
- Vaginal childbirth
- Ageing
- Menopause and oestrogen deficiency
- Prior pelvic surgery
- Increased intra-abdominal pressure:
- Chronic cough (e.g. COPD)
- Obesity
- Chronic constipation or straining
Pathophysiology
Loss of support from ligaments and connective tissue allows descent of pelvic organs, resulting in different types of prolapse:
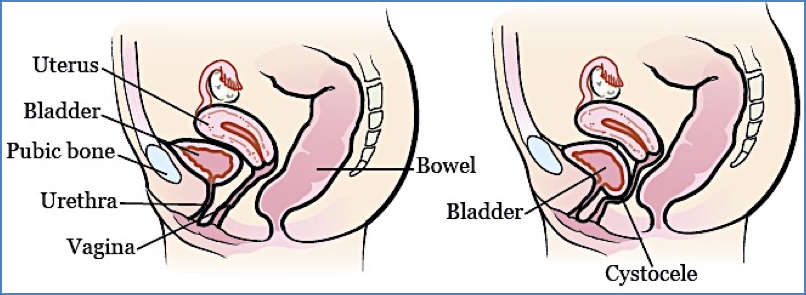
Anterior Prolapse
Cystocele / Cystourethrocele
- Bladder (± urethra) prolapses into the anterior vaginal wall
- Symptoms:
- Urinary frequency, urgency, nocturia
- Stress incontinence
- Urinary retention
- Recurrent urinary tract infections

2. Available from: https://www.researchgate.net/figure/Anterior-vaginal-wall-mass-mimicking-a-cystocele_fig2_43341879
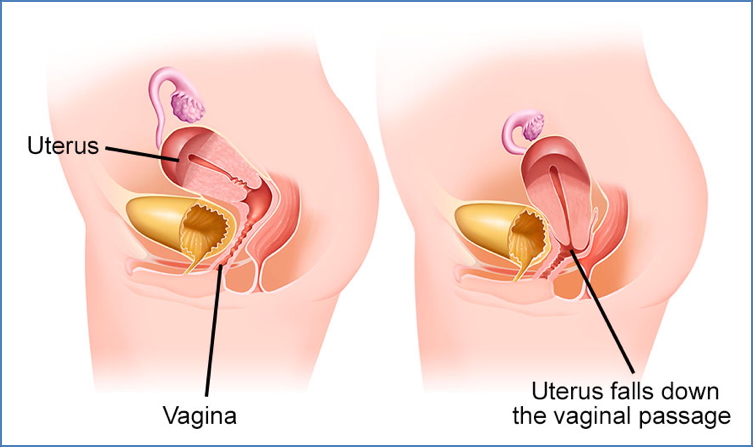
Uterocervical Prolapse
- Descent of the uterus, cervix, or vaginal vault (post-hysterectomy)
- Graded into 3 stages:
- Stage 1: Prolapse within vaginal canal
- Stage 2: Prolapse at level of introitus
- Stage 3: Prolapse beyond the introitus
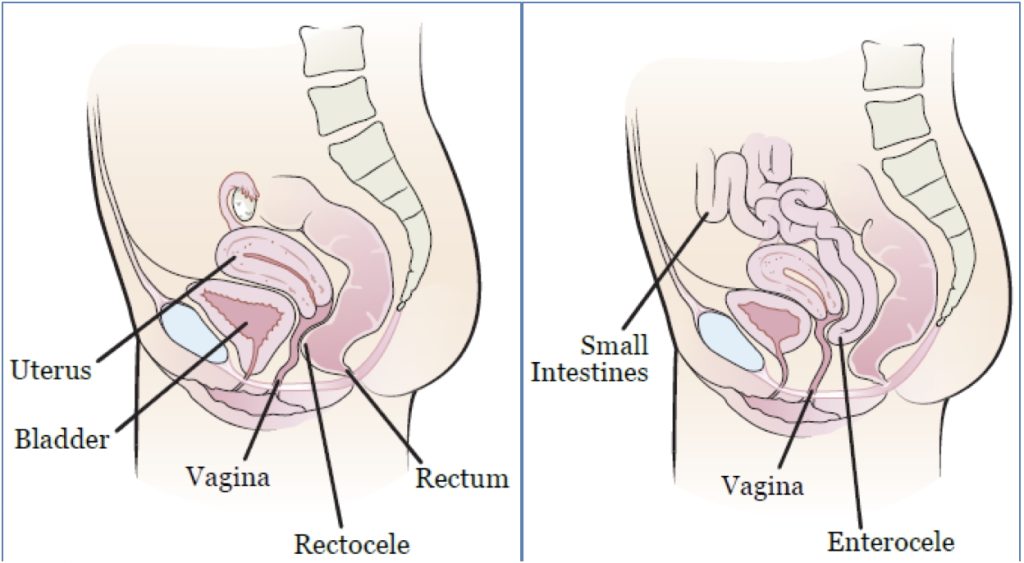
Posterior Prolapse
Rectocele
- Rectum bulges into the posterior vaginal wall
- Leads to constipation and difficulty with defecation
- Patients may manually reduce rectocele to evacuate
Enterocele
- Small intestine descends through the Pouch of Douglas into posterior vaginal wall
Clinical Features
Symptoms
- Pelvic heaviness, dragging, or fullness
- Worse on standing or lifting; relieved by lying down
- Referred lower back pain
- Dyspareunia and sexual dysfunction
- Urinary:
- Frequency, urgency, nocturia
- Stress incontinence
- Retention
- UTIs
- Constipation (especially in rectocele)
Signs
- Visible/palpable bulge at vaginal introitus
- Palpable bladder if urinary retention
- May observe signs of incontinence
Investigations
- Clinical diagnosis via speculum and bimanual pelvic examination
- Imaging (CT or MRI):
- Used pre-surgically or to confirm extent
- Specialist referral: Gynaecology assessment is essential
Management
Non-Surgical Options
- Vaginal ring pessary (suitable for elderly or surgery-unsuitable patients)
- Topical or systemic oestrogen therapy
- Pelvic floor strengthening exercises (Kegel exercises)
- Laxatives if rectocele-associated constipation
Surgical Repair
- Anterior repair or sling: for cystocele or cystourethrocele
- Hysterectomy: for uterocervical prolapse
- Vault sling repair: for post-hysterectomy vault prolapse
- Posterior repair or sling: for rectocele and enterocele
Complications
- Incomplete bladder emptying → recurrent UTIs
- Incontinence (stress or urge)
- Bowel dysfunction
- Sexual dysfunction
- Ulceration or erosion of prolapsed tissues
Differential Diagnosis
- Vaginal mass (e.g. Gartner duct cyst, vaginal carcinoma)
- Urethral diverticulum
- Uterine fibroids protruding through the cervix
- Bladder or bowel pathology
Summary – Pelvic Organ Prolapse
Pelvic organ prolapse is the descent of pelvic organs into the vaginal canal due to weakening of pelvic floor structures. It presents with urinary, bowel, and sexual symptoms, often worsened by physical activity or prolonged standing. Diagnosis is clinical and management may be conservative or surgical depending on severity. For more, visit our Reproductive Health Overview page.