Table of Contents
Overview – Penile Malignancies
Penile malignancies, though rare in developed countries, are significant due to their association with high-risk human papillomavirus (HPV) subtypes and poor hygiene. Early dysplastic lesions such as erythroplasia of Queyrat and Bowen’s disease are precursors to invasive squamous cell carcinoma. Understanding their progression and clinical presentation is critical for early detection and effective treatment. This article outlines the key features of penile dysplasia and carcinoma, including their pathogenesis, morphology, and management strategies.
Definition
Penile malignancies include precancerous dysplasias (intraepithelial neoplasia) and invasive squamous cell carcinoma arising from the penile skin or mucosa, most commonly due to oncogenic HPV infections.
Aetiology
- HPV Types 16 & 18 → high-risk oncogenic strains
- Other Risk Factors:
- Phimosis
- Chronic inflammation and poor hygiene
- Smoking
- Possibly lack of circumcision (some evidence suggests a protective effect)
Pathogenesis
- Oncogenic HPV → Viral integration into host DNA
- → Inactivation of tumour suppressors (e.g. p53, Rb)
- → DNA damage → Epithelial dysplasia
- → If untreated: progression to squamous cell carcinoma
Morphology
Dysplastic Lesions
- Erythroplasia of Queyrat:
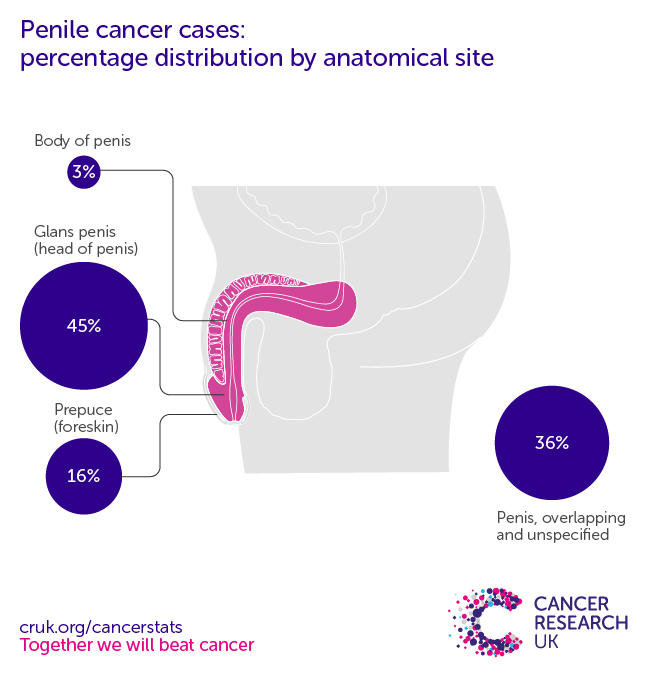
- In situ squamous dysplasia of the glans penis
- Appears as a red, velvety patch
- Bowen’s Disease:
- In situ dysplasia on the shaft of the penis
- Often scaly or crusted

Microscopy:
- Dysplastic epithelial cells without invasion
- Intact basement membrane
Invasive Carcinoma
- Macroscopic:
- Ulcerated or nodular mass
- May be indurated or friable
- Microscopic:
- Well-differentiated squamous cell carcinoma
- Keratinisation with epithelial pearls

Clinical Features
Dysplasia
- Typically asymptomatic
- Chronic non-healing lesion
- Red or scaly patches on the glans or shaft
- Premalignant – potential progression to invasive cancer
Invasive Carcinoma
- Symptoms:
- Redness, pain, ulceration, or bleeding
- Malodourous or non-healing penile lesion
- Signs:
- Palpable inguinal lymphadenopathy in metastatic spread
- Complications:
- Metastasis to inguinal → iliac lymph nodes
- Local tissue destruction
Investigations
- Clinical examination of penile lesions
- Biopsy for histological confirmation
- Imaging (CT/MRI) to assess lymphatic spread
- HPV typing (optional) for prognostic insight
Management
Dysplastic Lesions (Erythroplasia of Queyrat & Bowen’s)
- Topical agents:
- Imiquimod 5% cream
- 5-Fluorouracil
- Surgical excision if resistant to topical therapy
- Close surveillance to monitor for progression
Invasive Carcinoma
- Surgery is the mainstay:
- Wide local excision
- Partial or total penectomy for extensive disease
- Lymphadenectomy if nodal spread
- Adjuvant radiotherapy or chemotherapy for advanced/metastatic disease
Complications
- Local tissue destruction and ulceration
- Psychological and sexual dysfunction following surgery
- Regional and distant metastasis
- Treatment-related morbidity (e.g. lymphoedema after lymph node dissection)
Summary – Penile Malignancies
Penile malignancies most often arise from precancerous dysplasias such as erythroplasia of Queyrat and Bowen’s disease, both associated with HPV types 16 and 18. If left untreated, these lesions may progress to invasive squamous cell carcinoma, typically presenting as a non-healing ulcer or mass. Early identification and prompt treatment — including topical therapy, surgery, or adjuvant modalities — are essential. For broader context, see our Reproductive Health Overview page.