Table of Contents
Overview – Testicular Atrophy
Testicular atrophy refers to the progressive shrinkage and loss of function of the testicles. It can result from a range of chronic systemic, endocrine, or toxic causes, and is associated with infertility, increased cancer risk, and hormonal deficiency. Early recognition is important for investigating reversible causes and managing long-term complications.
Definition
Testicular atrophy is the decrease in size and function of one or both testicles, involving loss of spermatogenic activity and androgen production.
Aetiology
- Endocrine Causes:
- Hypopituitarism
- Chronic Systemic Illness:
- Chronic liver disease
- Chronic alcoholism
- Medical Interventions:
- Chemotherapy
- Radiation therapy
- Exogenous Hormones:
- Long-term anabolic steroid use
Pathogenesis
- Impaired endocrine or gonadal function →
- Loss of spermatogenesis
- Sertoli cell atrophy
- Leydig cell hyperplasia (compensatory)
- Leads to testicular shrinkage and compromised fertility/hormonal function
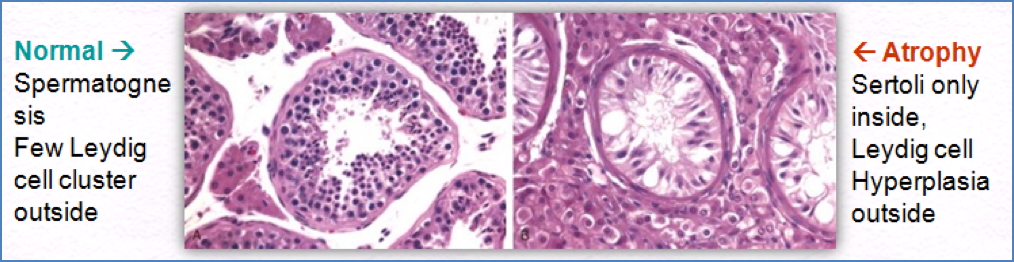
Morphology
- Macroscopically:
- Shrunken, firm testicle(s)
- May be unilateral or bilateral depending on the underlying cause

Clinical Features
- Often asymptomatic or discovered incidentally
- May present with:
- Decreased testicular volume
- Reduced libido
- Erectile dysfunction
- Infertility
Investigations
- Ultrasound scan – assess testicular size, echotexture, and blood flow
- Hormonal testing – LH, FSH, testosterone levels
- Urine/STI screening – especially in young or sexually active patients
- Tumour markers (if suspicious mass)
Complications
- ↑ Risk of Testicular Cancer
- ↑ Risk of Testicular Torsion
- Infertility
- Psychological impact
Management
- Treat underlying cause (e.g., stop steroids, treat liver disease)
- Hormone Replacement Therapy (HRT) – if low testosterone
- Fertility counselling – sperm banking, assisted reproduction if relevant
- Self-examination education – regular testicular self-assessment to detect cancer early
Summary – Testicular Atrophy
Testicular atrophy is a pathological shrinkage of testicular tissue due to systemic, endocrine, or iatrogenic causes, and may result in infertility, hormonal dysfunction, or increased cancer risk. Management focuses on addressing underlying causes, hormone replacement if needed, and cancer screening. For a broader context, see our Reproductive Health Overview page.