Table of Contents
Overview – COPD
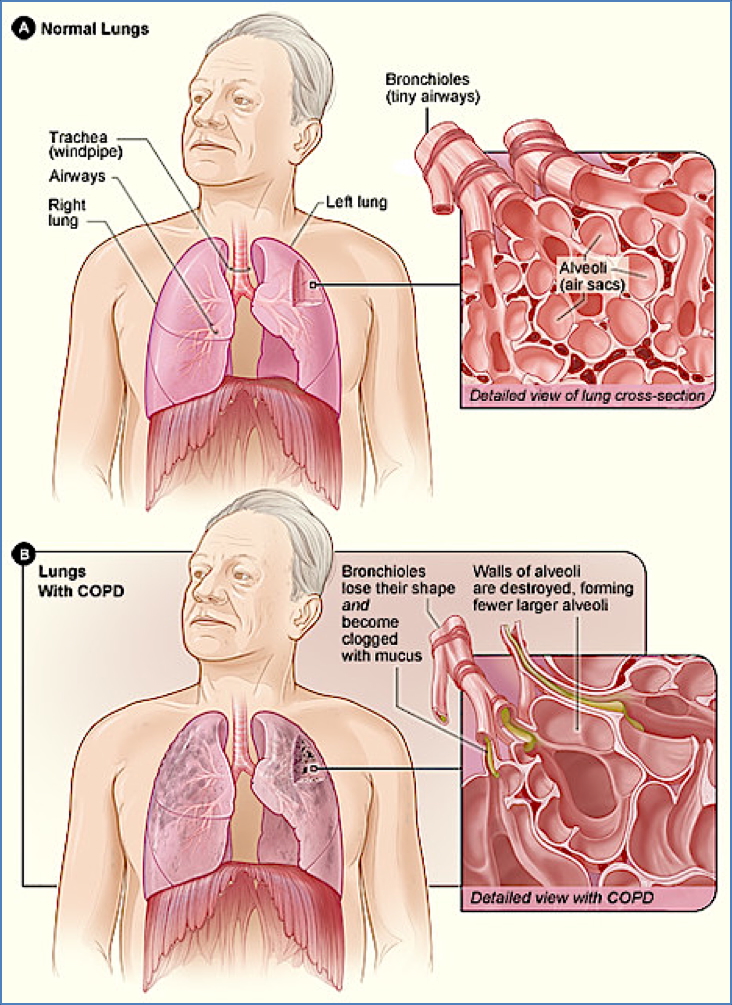
Chronic Obstructive Pulmonary Disease (COPD) is an umbrella term for a group of progressive respiratory conditions that cause airflow limitation due to airway or alveolar abnormalities. Primarily caused by long-term exposure to noxious particles, particularly tobacco smoke, COPD includes chronic bronchitis and emphysema. It is a major global cause of morbidity and mortality, commonly presenting with cough, dyspnoea, and sputum production.
Definition
COPD is characterised by persistent, largely irreversible airflow limitation due to chronic inflammation of the airways and lung parenchyma.
Aetiology
- Primary Risk Factor: Smoking (most significant)
- Other Causes:
- Environmental pollution
- Occupational exposures
- Genetic: α1-antitrypsin deficiency (esp. in early-onset emphysema)
Pathophysiology
Mechanisms of Airflow Obstruction:
- Within the airway lumen – e.g., mucus hypersecretion
- Within the airway wall – e.g., inflammation, oedema, bronchoconstriction
- External to the airway – e.g., loss of alveolar support in emphysema
This leads to:
- ↑ Airway resistance
- ↓ Elastic recoil
- Air trapping and hyperinflation
Clinical Features
General COPD Features:
- Exertional dyspnoea
- Chronic productive cough
- Wheezing
- Progressive exercise intolerance
Type A – “Pink Puffer” (Predominantly Emphysema):
- Dyspnoea with minimal cough
- Thin, barrel-chested appearance
- Quiet breath sounds
- Minimal cyanosis
- Near-normal arterial blood gases
Type B – “Blue Bloater” (Predominantly Chronic Bronchitis):
- Productive cough
- Cyanosis (hypoxaemia, hypercapnia)
- Coarse breath sounds with crackles
- Signs of right heart failure (e.g., peripheral oedema)

Investigations
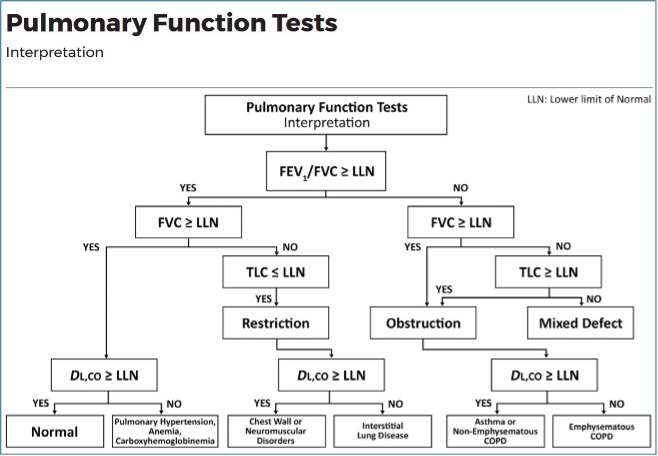
- Spirometry (Diagnostic gold standard):
- ↓ FEV₁/FVC ratio <70%
- ↓ FEV₁ (<80% of predicted)
- ↓ PEFR
- CXR:
- Hyperinflated lungs, flattened diaphragms
- Bullae (especially in emphysema)
- ABG: Hypoxia, hypercapnia (in severe cases)
- Full blood count: Possible polycythaemia
- α1-antitrypsin levels: If early-onset or family history
Management
Chronic (Stable) COPD:
- Smoking cessation (most important intervention)
- Bronchodilators:
- Antimuscarinics (e.g., ipratropium, tiotropium)
- β2-agonists (e.g., salbutamol, eformoterol)
- Inhaled corticosteroids (e.g., fluticasone, budesonide)
- Vaccination:
- Pneumococcal (Pneumovax)
- Annual influenza (Fluvax)
- Pulmonary rehabilitation: Exercise training and education
- Oxygen therapy (if chronic hypoxaemia)
- Diuretics: For cor pulmonale
Acute Exacerbations:
- Short-acting bronchodilators
- Oral/IV corticosteroids
- Empirical antibiotics (e.g., doxycycline, amoxicillin-clavulanate)
- Theophylline (as needed)
- Consider non-invasive ventilation or mechanical ventilation in severe cases
Complications
- Acute infective exacerbations
- Cor pulmonale (right heart failure)
- Polycythaemia
- Pneumonia
- Lung cancer
- Respiratory failure
- End-stage disease requiring palliative oxygen therapy
Subtypes of COPD
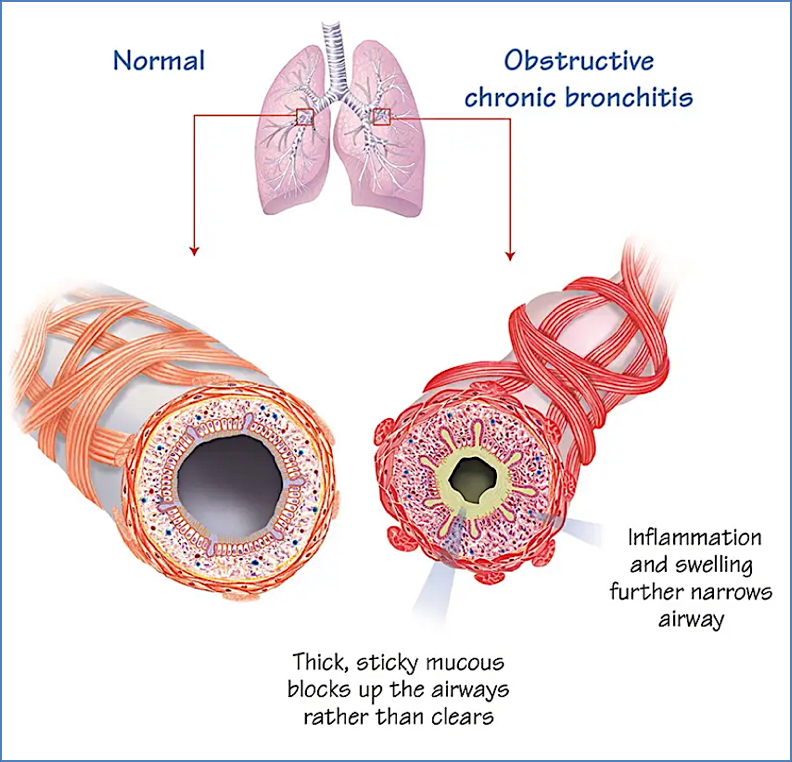
Chronic Bronchitis
Definition: Chronic productive cough lasting >3 months per year for >2 consecutive years.
Pathogenesis:
- Chronic inflammation from smoking/pollution
- Mucous gland hyperplasia → excess mucus
- Reduced ciliary function → mucus retention and infection
Clinical Features:
- Productive cough, cyanosis
- Wheeze, recurrent infections
- Peripheral oedema, obesity
Investigations:
- Spirometry: ↓ FEV₁/FVC ratio
- CXR: Hyperinflation, bronchial markings
- ABG: ↑ CO₂, ↓ O₂
Management:
- Same as general COPD, with emphasis on infection control and mucus clearance
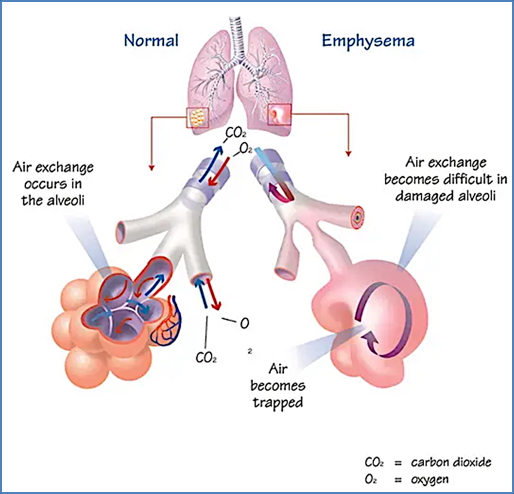
Emphysema
Definition: Permanent enlargement of alveolar spaces with alveolar wall destruction.
Types:
- Centrilobular: Most common, smoking-related
- Panacinar: Linked to α1-antitrypsin deficiency
Pathogenesis:
- Smoking → free radicals → elastase/protease activity → alveolar wall destruction
Clinical Features:
- Dyspnoea, minimal cough
- Barrel chest, hyperresonant chest
- Pursed-lip breathing
- “Pink Puffer” appearance
Investigations:
- Spirometry: ↓ FEV₁, ↑ TLC, ↓ DCo
- CXR: Hyperinflation, bullae
- α1-antitrypsin screen
Management:
- Similar to general COPD
- Genetic counselling if α1-antitrypsin deficiency

Summary – COPD
COPD is a progressive, largely irreversible respiratory disease characterised by airflow limitation due to chronic bronchitis, emphysema, or both. Smoking is the most important risk factor, and patients may present with chronic cough, dyspnoea, or wheeze. Diagnosis is confirmed by spirometry, and treatment involves smoking cessation, inhaled therapies, vaccinations, and oxygen for advanced cases. For broader context, visit our Respiratory Overview page.