Table of Contents
Overview – Hyperbaric & Hypobaric Physiology
Hyperbaric and hypobaric physiology examines how changes in barometric pressure affect gas exchange, breathing, and organ function. At altitude, reduced barometric pressure leads to hypoxia, while underwater, increased pressure alters gas solubility and volume. These shifts explain important clinical and physiological phenomena such as nitrogen narcosis, decompression sickness, acute mountain sickness, and high-altitude pulmonary oedema. Understanding these principles is vital for aviation medicine, diving medicine, and critical care.
Basics of Hyper/Hypo-Baric Conditions
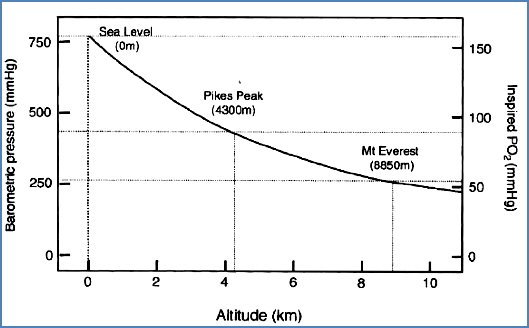
- Barometric pressure falls with altitude.
- Oxygen concentration remains constant at ~21%.
- Partial pressure of water vapour remains constant at 47 mmHg.
- Barometric pressure rises with depth.
- Each 10 metres underwater increases pressure by 1 atmosphere (~760 mmHg).
Gas Laws
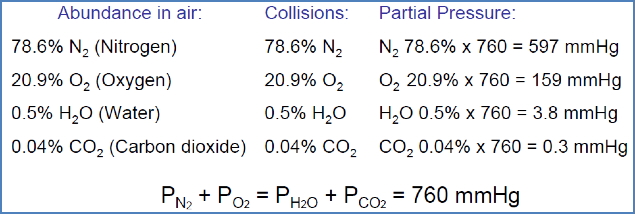
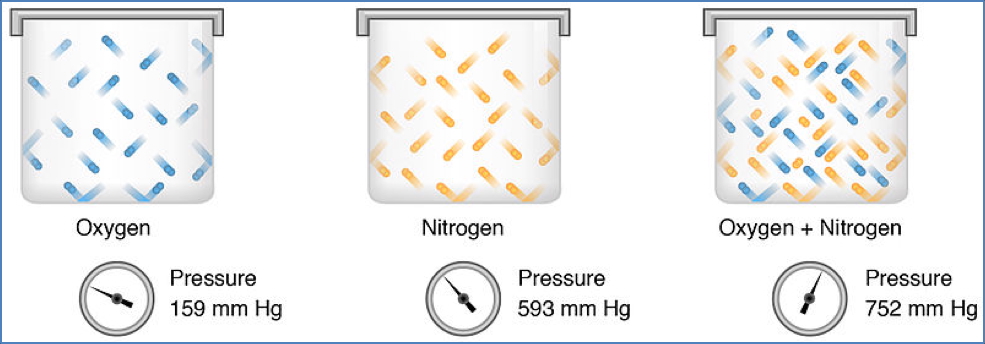
Dalton’s Law of Partial Pressures
- Total pressure of a gas mixture equals the sum of each component’s partial pressure.
- Partial pressure is proportional to its percentage composition.
Boyle’s Law (Pressure–Volume)
- At constant temperature, pressure is inversely proportional to gas volume.

Henry’s Law (Gas Dissolution)
- At constant temperature, the amount of dissolved gas is proportional to its partial pressure and solubility.

Hyperbaric Conditions (e.g. SCUBA Diving)
Gas Law Implications
- Dalton’s Law: Increased ambient pressure → increased partial pressures of gases.
- Boyle’s Law: Increased pressure → decreased gas volume.
- Henry’s Law: Increased pressure → more gas dissolves in body fluids.
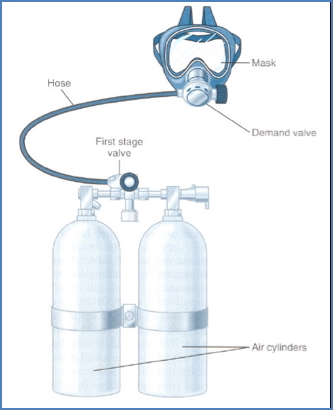
Breathing Apparatus
- Compressed air tanks supply gas at sufficient pressure.
- Regulator reduces pressure before inhalation.
- Mouthpiece with one-way valve.
- Minimal dead space tubing to reduce re-breathing of carbon dioxide.
Effects of High Partial Pressures of Oxygen
- Acute oxygen toxicity:
- At ~80 m depth, inspired PO₂ may reach 1500 mmHg.
- 1500 mmHg → oxygen poisoning.
- 3000 mmHg → seizures and coma.
- Pathophysiology:
- Brain highly sensitive to high PO₂.
- Excess O₂ forms free radicals → cellular injury.
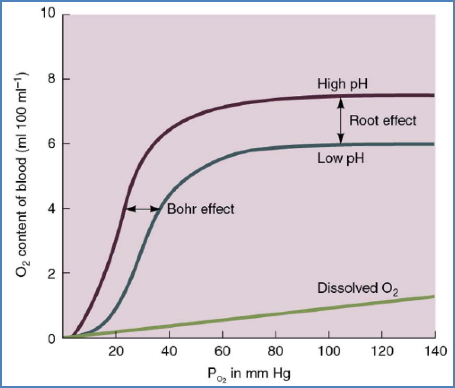
- Dissolved O₂ rises above haemoglobin’s functional range, rendering haemoglobin saturation redundant.
Effects of High Partial Pressures of Carbon Dioxide
- CO₂ usually regulated by metabolism rather than environment.
- Hypercapnia occurs if CO₂ accumulates in dead space and is re-breathed.
- Tolerable PCO₂ up to ~80 mmHg with increased respiratory drive.
- 80 mmHg → respiratory acidosis.
Effects of High Partial Pressures of Nitrogen
- Nitrogen narcosis:
- Nitrogen is lipid soluble.
- High partial pressures → neurological effects similar to alcohol intoxication (“raptures of the deep”).
- Decompression sickness (the bends):
- Rapid ascent → drop in pressure → nitrogen bubbles form in tissues and blood.
- Bubbles enlarge and block vessels → air emboli.
- Clinical effects:
- Joint and muscle pain.
- Paralysis, unconsciousness.
- Tissue ischaemia, infarction.
- Pulmonary haemorrhage (“the chokes”).
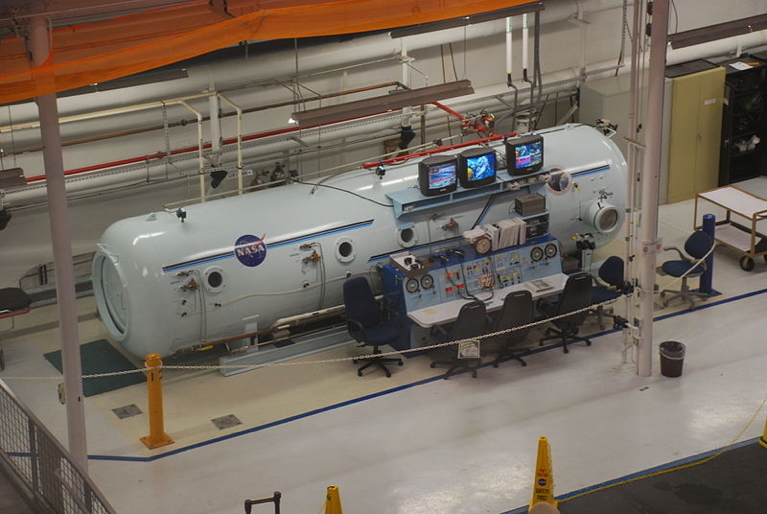
- Treatment: Hyperbaric recompression chamber.

Hypobaric Conditions (e.g. High Altitude)
Hypoxia
- Reduced barometric pressure → lower inspired PO₂.
- Decreases alveolar and arterial PO₂.
- Arterial PCO₂ decreases slightly at altitude due to hyperventilation.

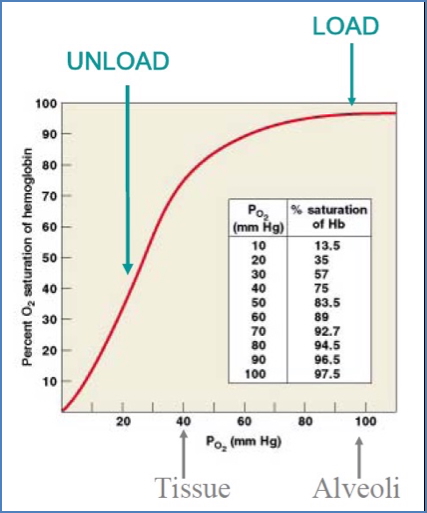
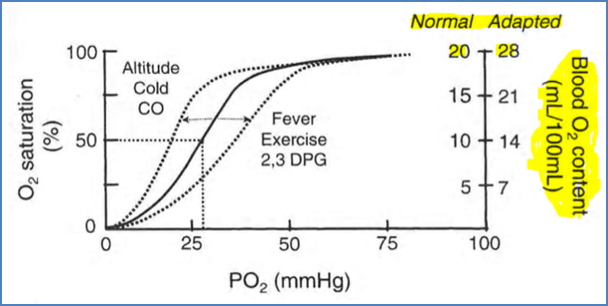
Haemoglobin–Oxygen Saturation
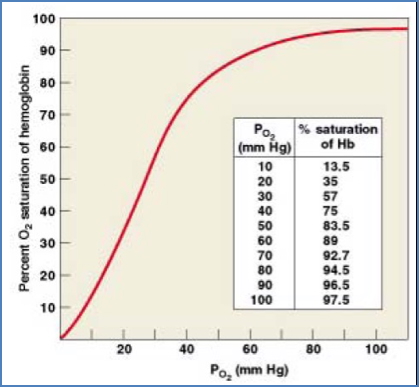
- Sea level: PO₂ ~160 mmHg → HbSat ~95%.
- 10,000 ft: PO₂ ~110 mmHg → HbSat ~90%.
- Above this: rapid fall in Hb saturation.
- Water vapour exerts relatively greater pressure at altitude, further reducing PO₂.
- HbSat stabilises at ~60–65% due to hyperventilation-induced alkalosis → left shift of Hb curve → improved O₂ loading.
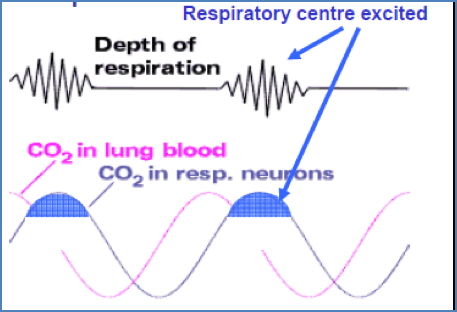
Cheyne–Stokes Breathing at Altitude
- Hypoxaemia (<60 mmHg) stimulates peripheral chemoreceptors → hyperventilation.
- Excess ventilation ↓ CO₂ → respiratory alkalosis → suppresses medullary chemoreceptors.
- Respiratory drive falls → hypoxaemia worsens → cycle repeats.

Effects of Hypoxia
- ~12,000 ft: impaired cognition, memory, motor skills; drowsiness; fatigue; nausea; euphoria.
- ~18,000 ft: twitching, seizures.
- ~23,000 ft: coma, death.
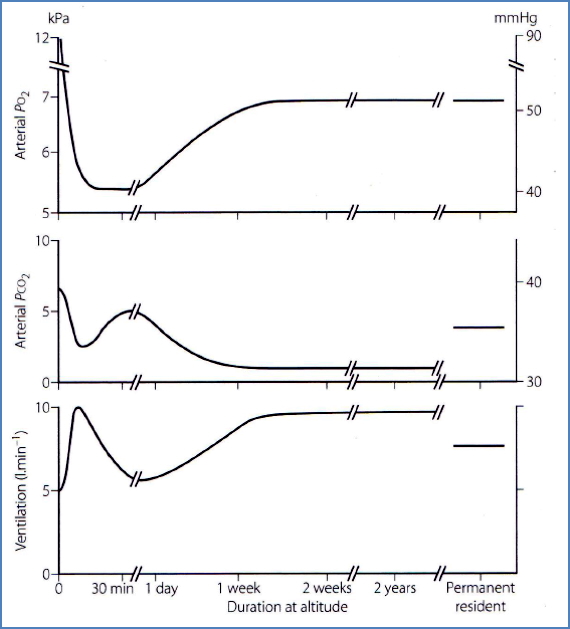
Acclimatisation
- Acute: ↑ ventilation, ↓ CO₂.
- Days: sustained hyperventilation, renal bicarbonate excretion compensates alkalosis.
- Chronic:
- ↑ erythropoiesis → ↑ red blood cell count and O₂-carrying capacity.
- Angiogenesis in lungs and tissues → improved perfusion.
- Enhanced aerobic metabolism efficiency.
Altitude Pathologies
Acute Mountain Sickness (AMS)
- Typically occurs in individuals who ascend to high altitude too rapidly, before the body has time to adapt.
- Triggered by hypoxia due to reduced barometric pressure and oxygen availability.
- Common above 2,500 metres (8,200 ft), but risk increases with faster ascent and higher elevations.
- Symptoms usually appear within 6–12 hours of ascent and can include:
- Headache (most consistent early symptom)
- Nausea, anorexia
- Dizziness, insomnia
- Fatigue, malaise
- If uncorrected, can progress to HACE or HAPE.
- Management:
- Immediate descent is the definitive treatment.
- Supplemental oxygen and acetazolamide (carbonic anhydrase inhibitor) may help in mild to moderate cases.
- Untreated, AMS can be fatal due to progression to life-threatening complications.
High-Altitude Cerebral Oedema (HACE)
- A severe, life-threatening complication of AMS.
- Caused by vasodilation of cerebral vessels in response to hypoxia, leading to brain swelling (cytotoxic and vasogenic oedema).
- Often develops after several days at altitude >3,000–4,000 metres.
- Symptoms:
- Intense headache
- Altered mental status (confusion, disorientation)
- Ataxia (unsteady gait)
- Hallucinations and psychotic behaviour
- Decreased consciousness or coma in severe cases
- Management:
- Urgent descent is critical.
- High-flow oxygen therapy, dexamethasone, and hyperbaric bags may be used until evacuation is possible.
- Delay in treatment can lead to permanent brain injury or death.
High-Altitude Pulmonary Oedema (HAPE)
- A non-cardiogenic pulmonary oedema occurring at high altitudes, often independently or alongside AMS.
- Caused by hypoxia-induced pulmonary vasoconstriction, which increases pulmonary capillary pressure and leads to fluid leakage into alveoli.
- Typically develops within 2–5 days of rapid ascent to >2,500–3,000 metres.
- Symptoms:
- Persistent dry or productive cough (sometimes blood-tinged)
- Dyspnoea on exertion → progresses to dyspnoea at rest
- Tachycardia, tachypnoea
- Crackles on lung auscultation
- Cyanosis (late sign)
- Management:
- Immediate descent is essential.
- Supplemental oxygen, nifedipine, and rest are used acutely.
- Portable hyperbaric chambers may help in field settings.
Chronic Mountain Sickness (CMS)
- A maladaptive condition seen in individuals living at high altitude (>3,500 m) for extended periods.
- Characterised by excessive erythrocytosis due to chronic hypoxia → ↑ red blood cell mass → hyperviscosity.
- Symptoms:
- Headache, dizziness
- Cyanosis
- Pulmonary hypertension due to chronic hypoxic vasoconstriction
- Right ventricular hypertrophy → may progress to cor pulmonale (right-sided heart failure)
- Management:
- Descent to lower altitude is definitive.
- Phlebotomy, oxygen therapy, or acetazolamide may be used to manage symptoms in persistent cases.
Summary – Hyperbaric and Hypobaric Physiology
Hyperbaric and hypobaric physiology describes how barometric pressure shifts affect gas exchange and human function. Hyperbaric environments increase gas solubility, leading to risks such as oxygen toxicity, nitrogen narcosis, and decompression sickness. Hypobaric environments cause hypoxia, Cheyne–Stokes breathing, and altitude illnesses such as AMS, HACE, and HAPE. Adaptation occurs via hyperventilation, renal and haematological adjustments, and long-term tissue changes. For more on respiratory adaptations, see our Respiratory Overview page.