Table of Contents
Overview – Lower Airway Anatomy
The lower airway anatomy, beginning at the trachea and extending into the lungs, forms the respiratory zone where gas exchange occurs. These structures provide a large surface area for oxygen uptake and carbon dioxide removal, while also transitioning from the conducting passages of the upper airway into the alveoli. A solid grasp of lower airway anatomy is vital for understanding respiratory physiology, aspiration risks, and conditions such as asthma, bronchitis, and pneumonia.
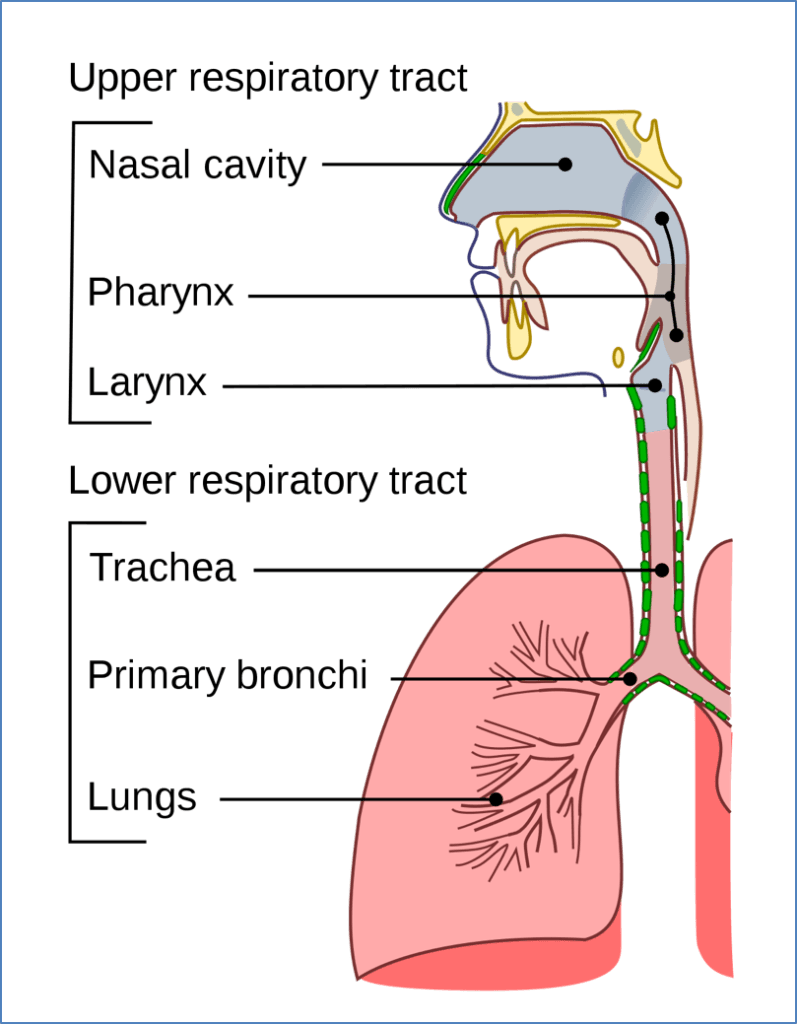
Structural Divisions
- Upper airways (conducting zone): nose → trachea
- Functions: filter debris, warm and moisten air
- Lower airways (respiratory zone): bronchi → lungs
- Functions: gas exchange (oxygen in, carbon dioxide out)
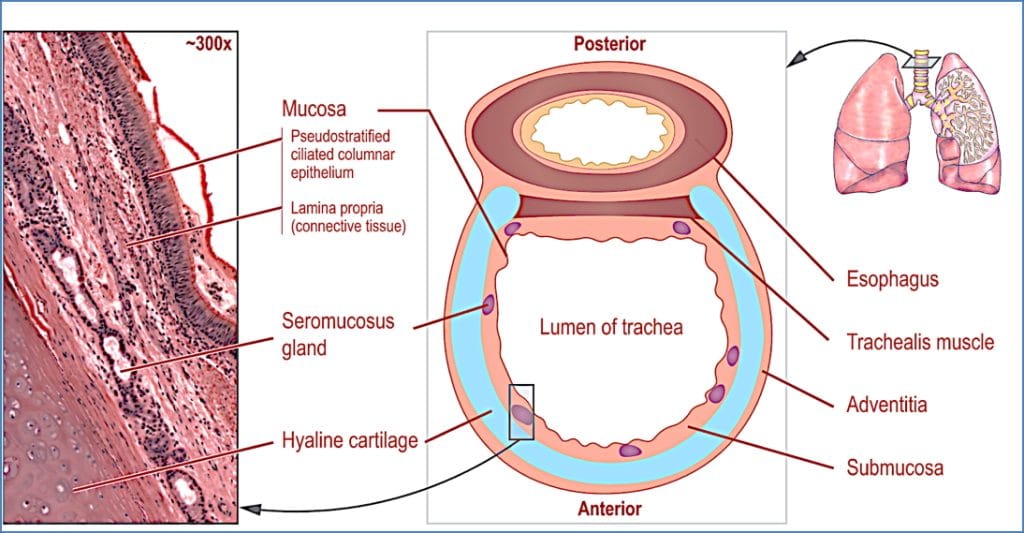
The Trachea
- Continuation of the pharynx
- Membranous tube of connective tissue and smooth muscle
- Reinforced by 15–20 C-shaped cartilage rings (incomplete posteriorly)
- Begins at C6 vertebra
- Terminates at bifurcation (carina) into bronchi at T4
- Right bronchus: more vertical than the left → inhaled objects more likely to lodge here
The Bronchial Tree
The bronchial tree refers to the branching network of airways within the lungs. It begins at the bifurcation of the trachea (T4 level), where it divides into:
- Right main bronchus (wider, shorter, more vertical → common site for aspirated objects)
- Left main bronchus (narrower, longer, more horizontal)
Each main bronchus divides into lobar bronchi (3 on the right, 2 on the left), then into segmental bronchi, which supply bronchopulmonary segments — the functionally independent units of the lung.
Gradual Structural Changes
As airways branch, they undergo structural adaptations:
- Cartilage: Complete rings → irregular plates → absent in bronchioles
- Epithelium: Pseudostratified columnar → simple columnar → simple cuboidal
- Cilia: Present in larger bronchi but sparse in distal bronchioles
- Smooth muscle: Increases relative to cartilage, aiding bronchiolar constriction/dilation
- Goblet cells: Decrease with depth; replaced by Clara (club) cells in terminal bronchioles
These changes help transition airflow from bulk conduction to finely regulated flow into the respiratory zone.

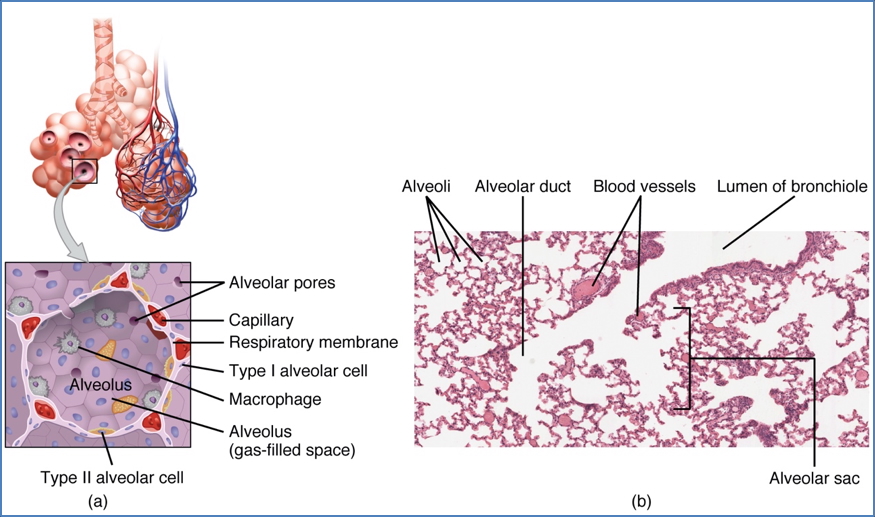
Respiratory Zone Anatomy
The respiratory zone begins at the level of the respiratory bronchioles, where alveoli start to appear along the walls. These lead into:
- Alveolar ducts (lined by alveoli)
- Alveolar sacs (clusters of alveoli)
Together, these structures form a massive surface area (~70 m²) for gas exchange.
Each alveolus is wrapped in a fine network of pulmonary capillaries, allowing oxygen and carbon dioxide to diffuse across the respiratory membrane — a thin barrier formed by:
- Alveolar epithelium (Type I cells)
- Capillary endothelium
- Shared basement membrane

Alveolar Cells
Type I Pneumocytes
- Make up ~95% of alveolar surface
- Very thin squamous cells
- Optimized for gas diffusion
- Terminally differentiated — not capable of repair
Type II Pneumocytes
- Cuboidal shape
- Produce pulmonary surfactant, a lipoprotein that reduces surface tension
- Prevents alveolar collapse during expiration
- Capable of mitosis — they regenerate both Type I and II cells after injury
Clinical Note – Surfactant
Surfactant production begins around week 26 of gestation and becomes sufficient by week 35. Deficiency causes neonatal respiratory distress syndrome (NRDS) — a life-threatening condition treated with surfactant replacement therapy and ventilatory support.
Functional Integration
The alveoli represent the endpoint of the respiratory tract and the primary site of gas exchange. Their architecture allows:
- Maximal surface area in minimal volume
- Short diffusion distances between air and blood
- Elastic recoil for efficient ventilation
- Interconnected pores of Kohn, which allow collateral ventilation between alveoli
Gas exchange efficiency depends on:
- Partial pressure gradients (O₂ in, CO₂ out)
- Surface area (destroyed in emphysema)
- Membrane integrity (thickened in pulmonary fibrosis)
- Perfusion matching (impaired in pulmonary embolism)
Review of Entire Respiratory Anatomy:

Summary – Alveolar and Lower Airways Anatomy
The lower airways anatomy helps conduct air from the bronchi into the alveoli, where gas exchange occurs. Bronchial epithelium transitions and cartilage loss mark the shift from conducting to respiratory zones. Alveoli are lined by Type I and II pneumocytes — the latter crucial for surfactant production. Understanding these microstructures is essential to grasp ventilation, diffusion, and common pathologies. For more on the respiratory system, visit our Respiratory Overview page.