Table of Contents
Overview – Neonatal Respiratory Transition
At birth, the infant must rapidly transition from placental to pulmonary gas exchange. This high-yield topic of the neonatal respiratory transition outlines the triggers for neonatal breathing, clearance of lung fluid, major circulatory shifts (including closure of fetal shunts), and postnatal lung growth. Also covered are key neonatal pathologies such as IRDS, SIDS, and meconium aspiration. Essential for paediatrics, obstetrics, and respiratory physiology.
Transition to Extra-Uterine Life
Initiation of Breathing
- Loss of placenta:
- Removes metabolic and respiratory support.
- Results in hypoxia and hypercapnia, stimulating the medullary respiratory centre.
- Breathing triggers:
- Hypoxia.
- Touch and skin cooling.
- Possible hormonal or chemical stimuli.
- Timing:
- First breath usually occurs within 20 seconds.
- Normal breathing rhythm is established by 90 seconds.
- Survival without breathing can extend to 10 minutes, but irreversible brain damage occurs after ~8 minutes.
- Maternal anaesthetics may delay the onset of breathing.
Removal of Lung Fluid
- At birth, alveolar epithelial cells switch from fluid secretion to absorption.
- Thoracic compression during vaginal delivery expels some of the lung fluid.
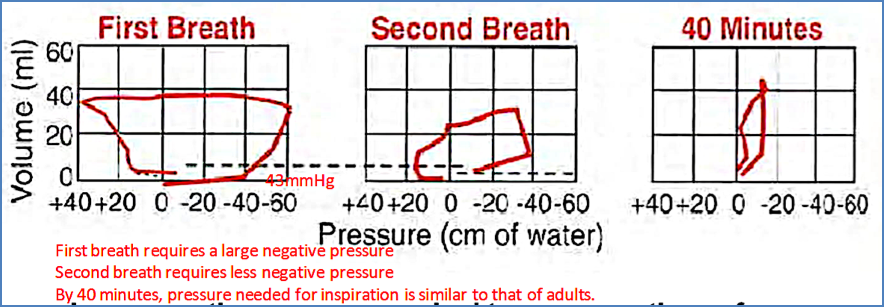
The First Breaths
- Remaining fluid causes high surface tension, demanding greater inspiratory effort.
- First breath: requires –25 to –40 mmHg pressure (vs. –15 mmHg in adults).
- Alveoli must remain partially inflated after the first breath to prevent collapse.
- Subsequent breaths: require less negative pressure.
- By 40 minutes: inspiratory effort is similar to that of adults.
Circulatory Readjustments
- Closure of foramen ovale:
- Placental loss → ↑ systemic vascular resistance → ↑ aortic, left atrial, and left ventricular pressures.
- Lung inflation → ↓ pulmonary vascular resistance → ↓ right atrial and right ventricular pressures.
- This pressure gradient closes the foramen ovale flap.
- Closure of ductus arteriosus:
- Drop in prostaglandins → contraction of ductus arteriosus smooth muscle → permanent closure.
Postnatal Lung Growth and Development
- Foetal haemoglobin: replaced by adult haemoglobin by 6 months.
- Alveoli: 50 million at birth → ~300 million in adulthood.
- Alveolar diameter: 0.15 mm → 0.3 mm.
- Surface area: 4 m² → 100 m².
- Lung volume: 250 mL → 5000 mL.
- Lung weight: 50 g → 800 g.
Neonatal Respiratory Disorders
Infant Respiratory Distress Syndrome (IRDS)
- Cause: Prematurity (<25 weeks) with insufficient surfactant.
- Consequences:
- ↑ alveolar surface tension.
- ↓ lung compliance (10–20% of normal).
- High inspiratory pressures required.
- Alveolar collapse (atelectasis), hypoxia, hypercapnia, hyaline membrane formation.
- Periodic or Cheyne–Stokes breathing due to immature respiratory centres.
- Treatment:
- Mechanical ventilation: CPAP (continuous positive airway pressure) or PEEP (positive end-expiratory pressure).
- Exogenous surfactant replacement (artificial or natural).
Sudden Infant Death Syndrome (SIDS)
- Definition: Death of an infant <1 year that remains unexplained, usually during sleep.
- Peak incidence: 2–3 months.
- Contributing factors: prematurity, low birth weight.
- Proposed mechanisms:
- Central apnoea from immature respiratory control.
- Abnormal thermoregulation (overheating risk).
- Prolonged apnoea episodes during periodic breathing.
- Anecdotal evidence of vaccine-related SIDS deaths (mechanism unknown)
Premature Rupture of Membranes
- Risk of Foetal Infection
- Lack of Mechanical Protection of baby
- Baby may be contorted – as there is no room to move with no amniotic fluid.
- Effects on Respiratory Development:
- Amniotic Fluid Aids in the Development of Lungs – If no fluid → Lung membranes become dry → Don’t grow properly → ↓Surfactant Production → IRDS.
Meconium Aspiration Syndrome
- Occurs when a fetus inhales meconium-stained amniotic fluid in utero or during delivery
- Common in post-term or distressed infants (due to hypoxia-induced meconium passage)
- Meconium → irritates airways, causes inflammation, infection risk, and airway obstruction
- Can lead to:
- Atelectasis (alveolar collapse)
- Chemical pneumonitis
- Pulmonary hypertension
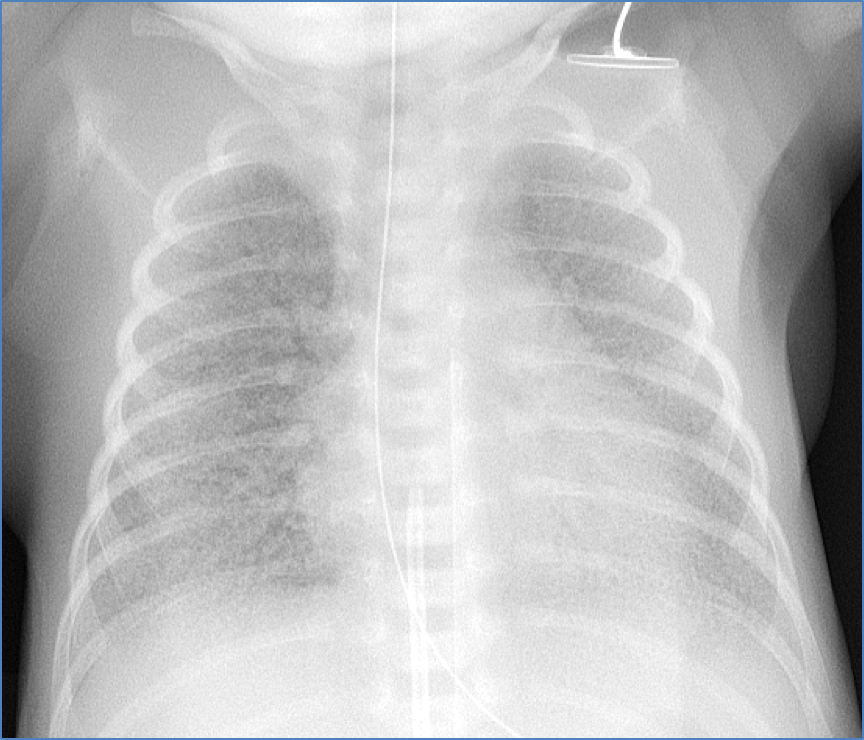
- CXR: patchy infiltrates, hyperinflation, flattened diaphragm
- Management:
- Supportive care (oxygen, ventilation)
- Surfactant therapy if needed
- ECMO in severe cases
Summary – Neonatal Respiratory Transition
Neonatal respiratory transition is a critical physiological shift involving the initiation of breathing, clearance of fetal lung fluid, and closure of circulatory shunts. Successful adaptation relies on surfactant, healthy respiratory control, and structural lung development. Conditions like IRDS and SIDS highlight the vulnerability of this transition period. For more, visit our Respiratory Overview page.