Table of Contents
Overview – Pneumonias
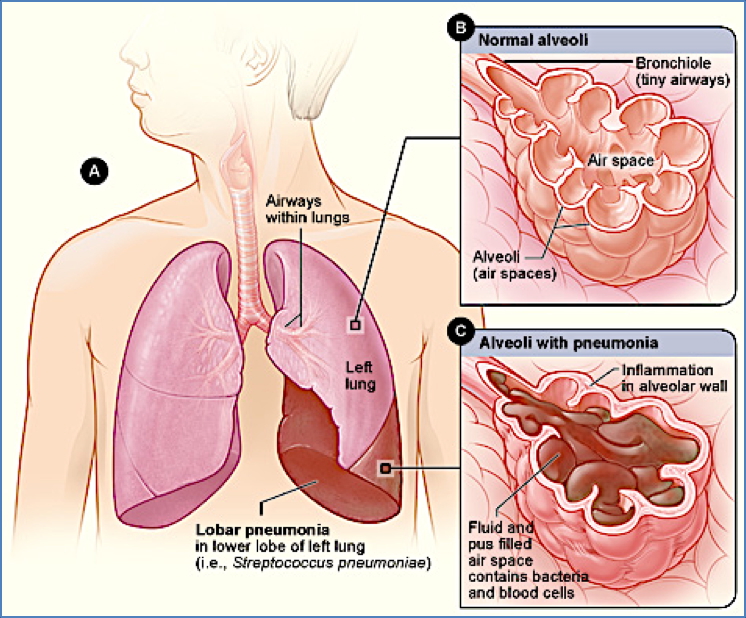
Pneumonias are infections of the lung parenchyma resulting in inflammation and consolidation of alveolar spaces. It can be classified based on its clinical setting (community-acquired, hospital-acquired, or atypical), as well as its morphological pattern (lobar, bronchopneumonia, or interstitial). Clinical features vary with the cause and type, but commonly include fever, productive cough, and dyspnoea. Prompt diagnosis and treatment are crucial to prevent complications such as sepsis, respiratory failure, and abscess formation.
Definition
Pneumonia refers to inflammation of the lungs, typically caused by infectious agents, resulting in alveolar consolidation and impaired gas exchange.
Aetiology
Community-Acquired Pneumonia (CAP)
- Common organisms:
- Streptococcus pneumoniae (90%)
- Haemophilus influenzae
Hospital-Acquired (Nosocomial) Pneumonia
- Usually occurs >48 hours after admission
- More likely to be Gram-negative organisms:
- Pseudomonas aeruginosa, E. coli, Klebsiella
Atypical / Interstitial Pneumonia (“Walking Pneumonia”)
- Intracellular bacteria:
- Mycoplasma pneumoniae, Chlamydia pneumoniae, Legionella, Coxiella burnetii
- Viruses:
- Influenza, RSV, SARS-CoV-2
Immunocompromised Hosts
- Cytomegalovirus
- Pneumocystis jirovecii
- Fungal: Candida, Aspergillus
Pathogenesis
Infectious agents infiltrate the lungs via inhalation, aspiration, or haematogenous spread. The resulting inflammatory response leads to alveolar exudation, consolidation, and impaired oxygenation. Morphological patterns of involvement help distinguish types of pneumonia.
Types of Pneumonia
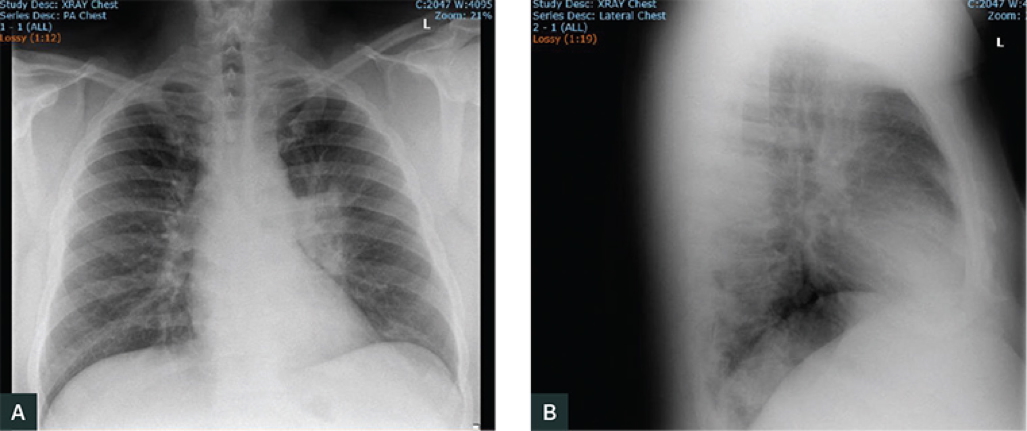
Lobar Pneumonia
- Aetiology: Typically Strep pneumoniae; Klebsiella in elderly
- Pathogenesis: Alveolar exudate fills an entire lobe → consolidation
- Morphology:
- Single-lobe involvement
- Dense opacity on CXR
- Clinical Features:
- Abrupt high fever and chills
- Productive cough ± rusty sputum
- Pleuritic chest pain and pleural rub
- Usually unilateral

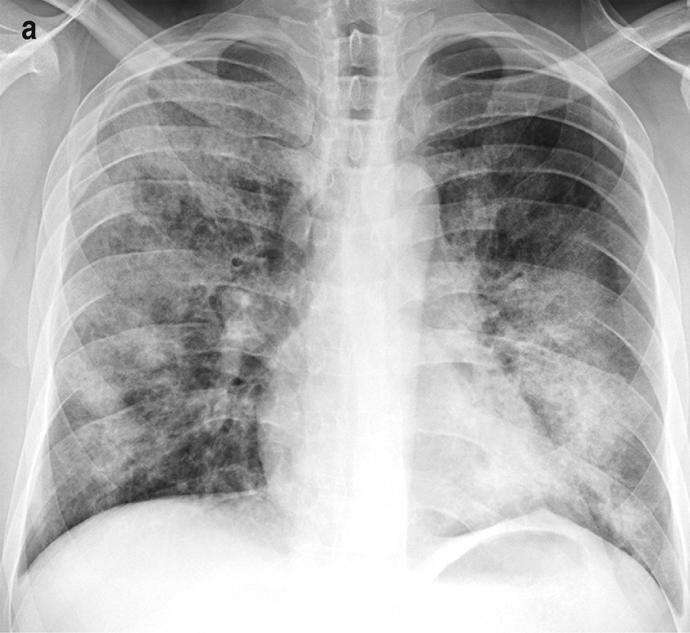
Bronchopneumonia
- Aetiology: Follows debilitating illness, surgery, or age extremes
- Strep pneumoniae, Staph aureus, H. influenzae
- Pathogenesis: Patchy, suppurative inflammation in multiple lobes
- Morphology:
- Multi-lobar and bilateral
- Patchy opacities on CXR
- Clinical Features:
- Similar to lobar pneumonia but more diffuse
- Often bilateral involvement
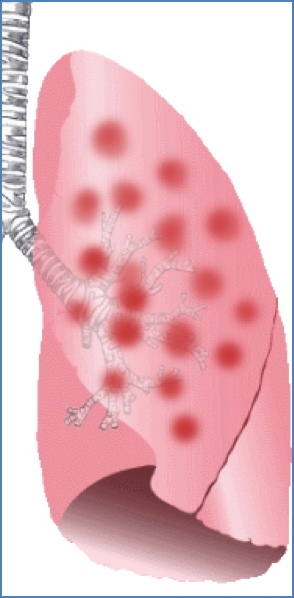
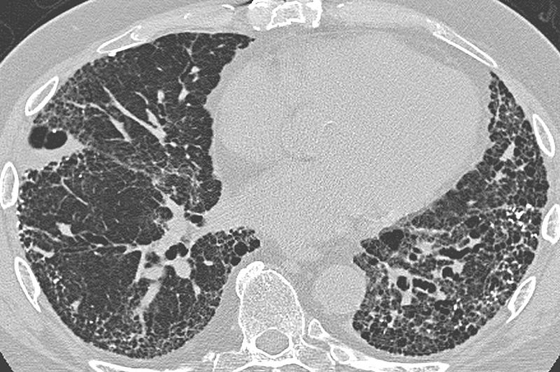
Atypical / Interstitial Pneumonia
- Aetiology:
- Bacteria: Mycoplasma, Chlamydia, Legionella, Coxiella
- Viruses: Influenza A/B, RSV, SARS-CoV-2
- Pathogenesis:
- Inflammation localised to alveolar septa/interstitium
- Lacks alveolar exudate
- Morphology:
- Diffuse interstitial pattern
- Typically bilateral
- Clinical Features:
- Gradual onset with flu-like symptoms
- Often non-productive cough
- Wheezing more common
- Lack of focal consolidation signs
Clinical Features of Pneumonias
General Pneumonia Triad (WHO)
- Fever
- Tachypnoea
- Tachycardia
Other signs:
- Pleuritic chest pain
- Dyspnoea or hypoxia
- Cough (productive or dry)
Investigations
- CXR: Determines distribution (lobar, patchy, interstitial)
- Sputum MCS / BAL / NPA
- Blood cultures if sepsis suspected
- Serology/PCR: Atypical organisms
- CURB-65 Score: For hospitalisation or ICU admission
Management of Pneumonias
Admission Criteria – CURB-65
- Confusion
- Urea >7 mmol/L
- Respiratory rate >30
- Blood pressure <90/60 mmHg
- Age >65 years
Score ≥3 → consider ICU admission
Antibiotics
Empirical Treatment
- Gram-positive: Amoxicillin, Benzylpenicillin, Doxycycline, Clarithromycin
- Gram-negative: Gentamicin, Ceftriaxone
- Severe: Consider Meropenem/Imipenem
Adjust based on culture sensitivity results.
Supportive Care
- IV Fluids
- Oxygen (if O₂ sats <92%)
- Antipyretics, analgesia
- Ventilatory support as needed
Complications
- ARDS – Severe hypoxia requiring mechanical ventilation
- Lung Abscess
- Pleuritis, Pleural Effusion, Empyema – Requires drainage + IV antibiotics
- Sepsis / Meningitis
- Fibrosis, scarring, adhesions
- Post-inflammatory bronchiectasis
- Rarely: Adenocarcinoma in scarred lung tissue
Summary – Pneumonias
Pneumonia is a common and potentially serious lung infection with diverse aetiologies and presentations. Accurate classification into lobar, bronchopneumonia, or atypical types aids diagnosis and management. Early intervention with antibiotics and supportive care can prevent serious complications like ARDS and empyema. For broader context, visit our Respiratory Overview page.