Table of Contents
Overview – Skin Appendages
Skin appendages are specialized structures that support the essential barrier, sensory, and homeostatic functions of the skin. These include vasculature, sensory receptors, glands, hair, and nails—all of which play critical roles in thermoregulation, environmental interaction, immunity, and hormonal response. Understanding the anatomy and physiology of skin appendages is vital for diagnosing and managing dermatological and systemic diseases. This article comprehensively explores the structure and function of skin appendages.
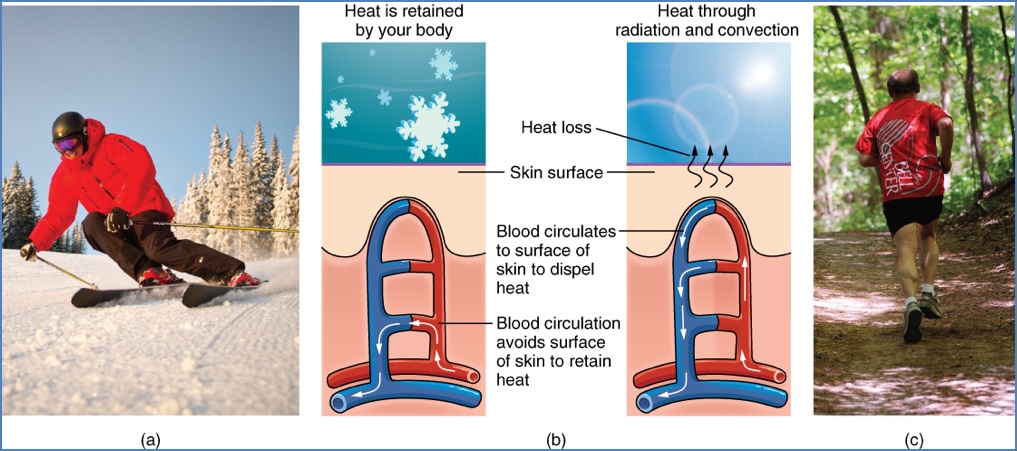
Vasculature
- Dermal vasculature: Dense capillary networks nourish the skin and aid in thermoregulation.
- Functions:
- Supplies nutrients to the skin
- Regulates body temperature via heat conduction and vasomotor changes
- Serves as a blood reservoir in times of circulatory stress (e.g. exercise, haemorrhage)
Cutaneous Circulatory Apparatus
- Nutritive vessels:
- Arteries, capillaries, veins
- Organized into a horizontal subdermal plexus
- Ascending arterioles branch into the subpapillary plexus in the papillary dermis
- Thermoregulatory vessels:
- Extensive subcutaneous venous plexi (hold large blood volumes)
- Arteriovenous anastomoses in high-heat-loss areas (hands, feet, lips, nose, ears)
Both systems are innervated by sympathetic adrenergic vasoconstrictor fibers, allowing modulation of blood flow and heat loss.
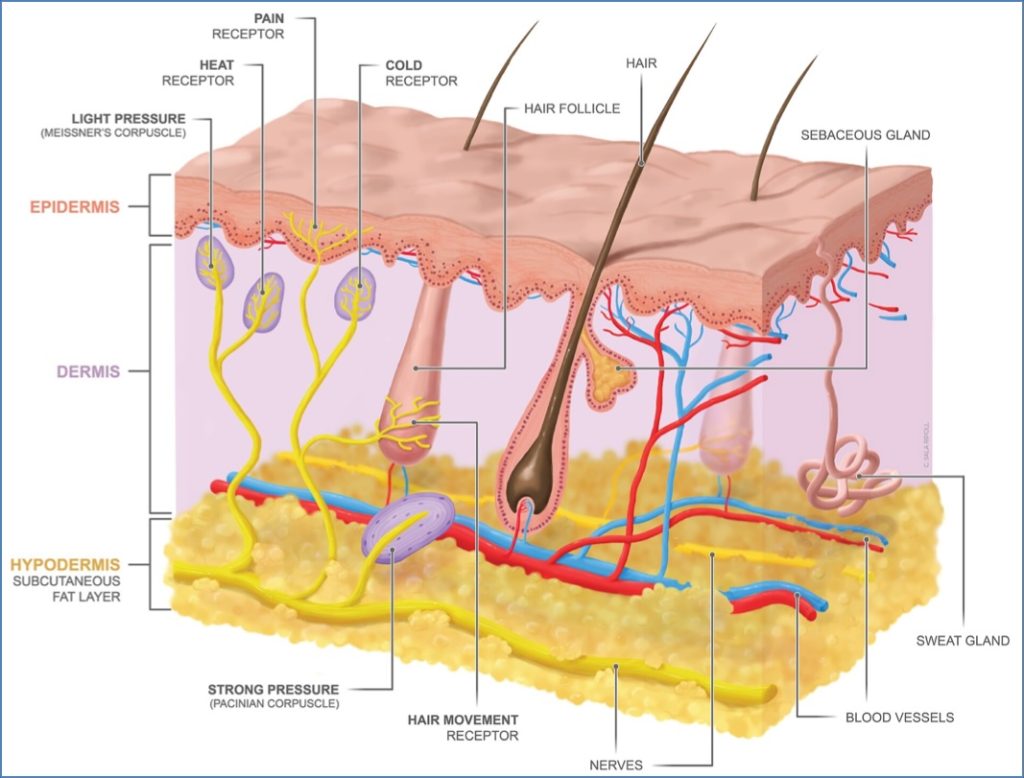
Sensory System
- Distribution: Densest in face and extremities; sparse on the back
- Function: Detects touch, pain, temperature, pressure, and itch
Types of Sensory Receptors
- Unencapsulated
- Free nerve endings: Pain, touch, temperature (in epidermis & superficial dermis)
- A-delta fibers: Myelinated, fast, sharp pain
- C-fibers: Unmyelinated, slow, dull, burning pain
- Merkel cell discs: Light touch (stratum basale)
- Hair-follicle receptors: Mechanoreceptors surrounding hair follicles
- Free nerve endings: Pain, touch, temperature (in epidermis & superficial dermis)
- Encapsulated
- Meissner corpuscles: Fine touch (dermal papillae)
- Pacinian corpuscles: Deep pressure (deep dermis/hypodermis)
- Ruffini endings: Stretch receptors (associated with collagen)
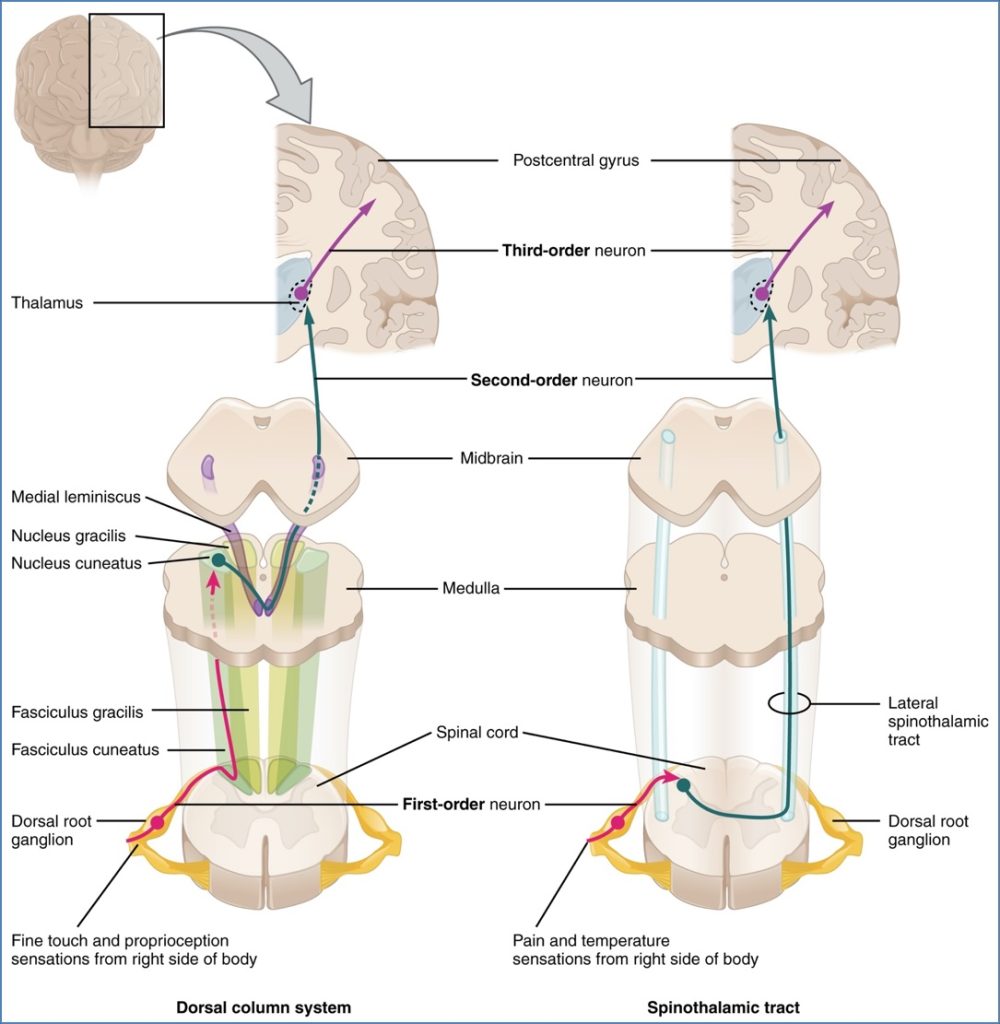
Sensory Pathway
- First-order neuron: DRG → dorsal horn of spinal cord
- Second-order neuron: Substantia gelatinosa → decussates → spinothalamic tract → thalamus
- Third-order neuron: Thalamus → internal capsule → sensory cortex
Receptor Physiology
- Adaptation: Decline in action potentials during constant stimulation
- Slow-adapting: Nociceptors
- Fast-adapting: Pacinian corpuscles
Glands
Sebaceous Glands
- Type: Holocrine
- Associated with: Hair follicles (pilosebaceous unit)
- Secretions: Sebum (triglycerides, wax esters, cholesterol) – antibacterial/antifungal
- Location: Absent on palms/soles; most abundant on face/scalp
- Hormonal control: Stimulated by androgens (↑ at puberty)
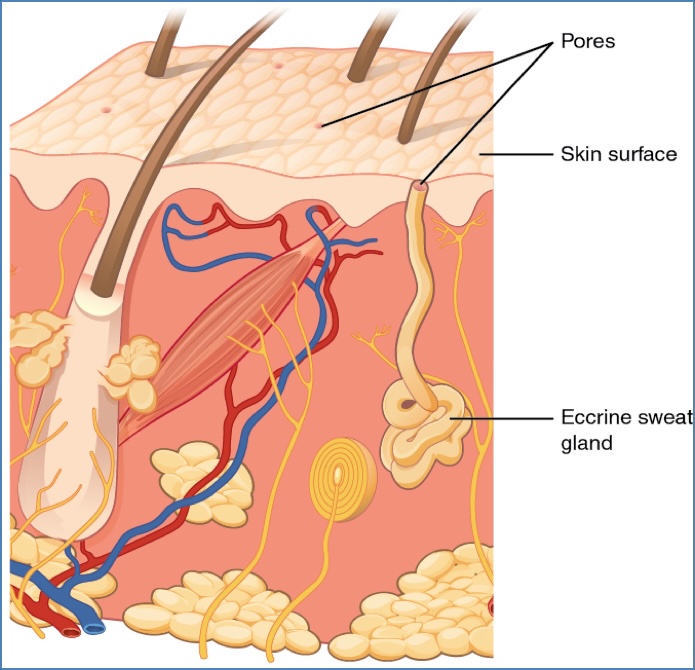
Eccrine Sweat Glands
- Type: Simple coiled tubular
- Location: Widespread (sparse on back)
- Function: Thermoregulation and emotional sweating
- Secretion of electrolyte-rich fluid → reabsorption of Na⁺ in duct
- Can excrete litres per hour
- Innervation: Sympathetic nervous system
Apocrine Glands
- Associated with: Hair follicles (axilla, groin)
- Location: Deep dermis
- Secretion: Milky, viscous fluid (proteins, cellular debris)
- Odour due to bacterial breakdown
- May play a pheromonal role
- Hormonal control: Stimulated by androgens, active post-puberty

Nails
- Composition: Dense keratinized plates
- Functions:
- Protect digits
- Assist in grasping
- Serve as sensory tools or weapons
Key Structures
- Nail plate: Fully keratinized, adherent to nail bed
- Nail bed: Skin beneath the nail plate
- Lunula: White crescent at base of nail
- Cuticle: Overlaps the nail at the proximal edge
- Nail matrix: Site of nail growth
- Paronychium: Skin around the nail
- Hyponychium: Distal nail edge detachment point
- Proximal & lateral nail folds: Protective skin borders

Hair & Pilosebaceous Unit
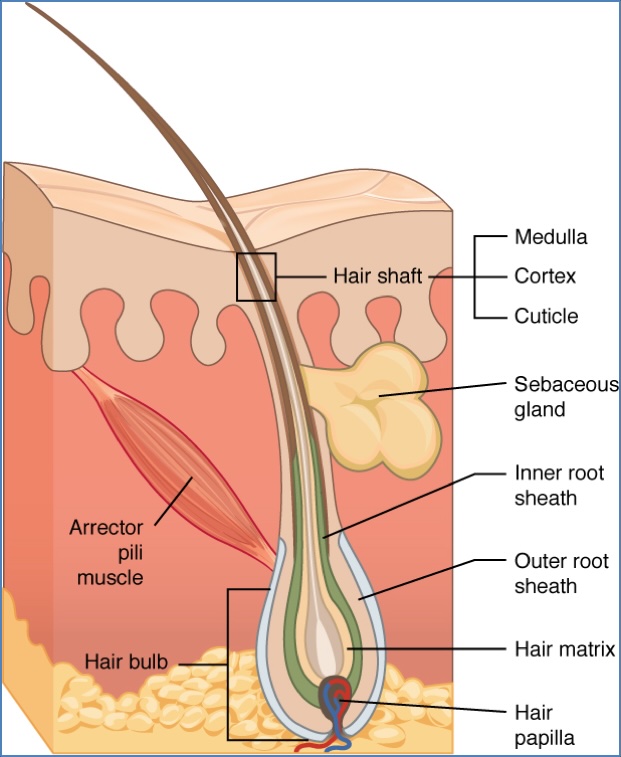
Structure
- Hair shaft + associated sebaceous and apocrine glands
- Arrector pili: Smooth muscle causing piloerection (goosebumps)
Hair Types
- Vellus: Fine, unpigmented (pre-pubertal and general body hair)
- Terminal: Thick, pigmented (scalp, beard, pubic areas)
Hormonal Regulation
- Androgen-sensitive: Hair transitions during puberty and aging
- Age-related changes: Terminal → vellus conversion on scalp
Hair Growth Cycle
- Anagen (growth): ~3 years – active keratinocyte proliferation
- Catagen (resting): ~2 weeks – programmed cell death
- Telogen (shedding): ~3 months – hair either sheds or is retained until next anagen phase
Hair Pigmentation
- Determined by melanocyte activity in anagen phase
- ↓ Melanin → greying
- Absent melanin → white hair
Summary – Skin Appendages
Skin appendages include glands, blood vessels, nerve endings, nails, and hair—each with distinct yet interconnected roles in sensory perception, thermoregulation, and protection. Their structure and function are key to understanding numerous dermatological and systemic diseases. This high-yield guide to skin appendages offers essential insight for medical students preparing for clinical placements and exams. For a broader context, see our Skin & Dermatology Overview page.