Table of Contents
Overview – Skin Healing
Skin healing is a complex, multi-phase biological process that restores skin integrity after injury. Understanding the causes of skin damage and the mechanisms of repair is essential for final-year medical students, as it underpins wound management, surgical planning, and treatment of skin diseases. This article provides a concise, high-yield guide to the causes of skin injury and the stages of skin healing. The term skin healing encompasses inflammation, granulation tissue formation, collagen deposition, and epithelialisation—key concepts for dermatology and clinical medicine.
Causes of Skin Injury
Physical Agents
- Mechanical trauma
- Burns (thermal)
- Cold injuries
- Electrical injuries
- Radiation (e.g. radiotherapy)
Hypoxia
- Ischaemic damage (e.g. peripheral vascular disease)
Chemical Exposure
- Acids and alkalis
- Phosphorus compounds
Infections
- Bacterial
- Viral
Autoimmune Conditions
- Scleroderma
- Systemic lupus erythematosus
Genetic Disorders
- Histiocytosis X
Mechanisms of Healing
Acute Inflammation
- Vasodilation → Increased local blood flow
- ↑ Vascular permeability → fluid stasis
- Leukocyte margination, adhesion, and migration
- Phagocytosis of debris and pathogens → enzyme release
Granulation Tissue Formation
- Develops 3–5 days post-injury (in deeper wounds only)
- Angiogenesis: Endothelial cell migration and proliferation
- Driven by:
- FGF (Fibroblast Growth Factor)
- VEGF (Vascular Endothelial Growth Factor)
- Driven by:
- Fibrosis: Fibroblast migration and collagen synthesis
- Driven by:
- PDGF (Platelet-Derived Growth Factor)
- TGF-β (Transforming Growth Factor Beta)
- Driven by:
Collagen Synthesis
- Structural protein forming the scaffold of repair
- Requires Vitamin C for hydroxylation during synthesis
- Strengthens gradually:
- Week 1: weak scar
- Peak tensile strength: ~3 months
- Matrix Metalloproteinases (e.g. collagenases, gelatinases) degrade and remodel collagen

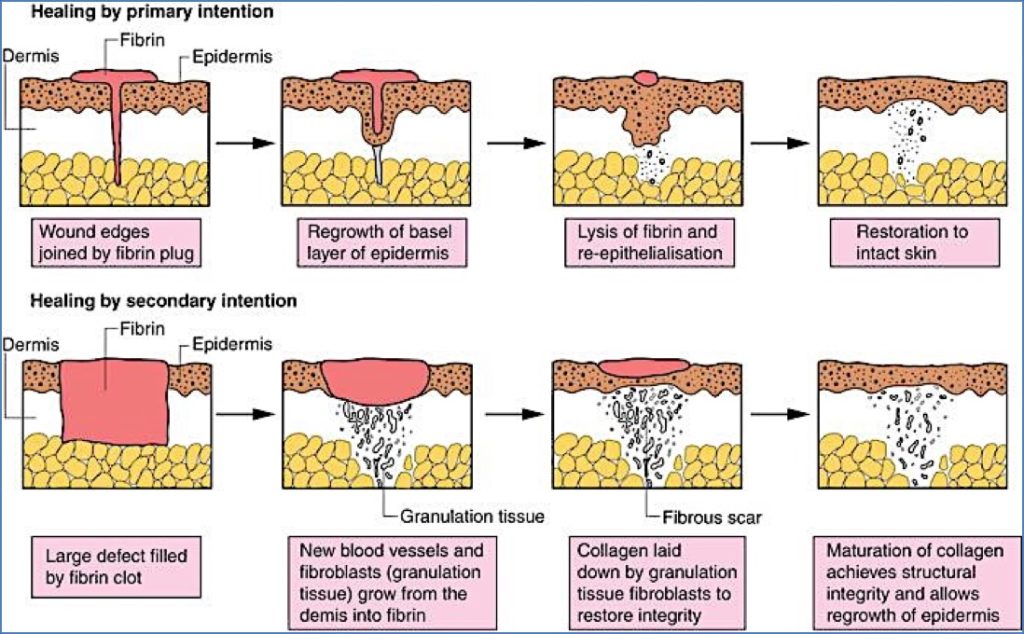
Healing by Primary vs Secondary Intention
Primary Intention
- Wound edges are closely apposed
- Minimal granulation tissue
- Rapid healing
- Re-epithelialisation occurs via basal layer cells within 1–2 days
Secondary Intention
- Larger, gaping wounds
- More extensive granulation tissue formation
- Slower process
- Epithelial cells proliferate from wound margins to cover defect
Summary – Skin Healing
Skin healing is a vital physiological process, involving inflammation, granulation tissue formation, collagen synthesis, and either primary or secondary intention closure. Whether the wound heals quickly or slowly depends on the wound characteristics and depth. A clear understanding of skin healing mechanisms helps guide treatment and optimize wound care in clinical practice. For more foundational content, see our Skin & Dermatology Overview page.